Learning Objectives
1. Demonstrate that Tolosa-Hunt syndrome is a diagnosis of exclusion
2. Evaluate the relative risks and benefits of invasive biopsy compared to imaging studies in diagnosis of a soft-tissue mass
3. Recognize perineural invasion as a potential route of invasive skin cancer
Case Description
A 65-year-old right-handed man with a history of right trigeminal neuralgia and basal cell carcinoma presented to the ED with one week of right ptosis and diplopia. He reported right-sided headache but denied trauma, nausea, or vomiting. Surgical history was significant for Mohs micrographic excision of squamous cell carcinoma of the right cheek in 2004, basal cell carcinoma of the mid forehead in 2004 and right forehead in 2016, right rhizotomy in 2018 and microvascular decompression 6 months prior to presentation. The decompression improved his trigeminal neuralgia symptoms, but left him with chronic sinusitis and anosmia, for which he received multiple CT scans and antibiotic courses. He reported a poor appetite and 30-lb. weight loss due to anosmia. Motor strength, sensation, coordination, and speech were intact on neurological exam. He displayed right-sided ophthalmoplegia with limited abduction, upward and downward gaze consistent with an oculomotor nerve palsy.
Non-contrast head CT scan revealed no intra-cranial hemorrhage. CT angiogram and venogram showed no vascular abnormalities but revealed an enhancing mass along the right cavernous sinus, measuring ~2.1x1.1cm. MRI confirmed the presence of enhancing soft tissue in the right cavernous sinus, extending into the foramen ovale (Figure 1).
Chest-abdomen-pelvis CT found no evidence of malignancy. CBC, serum chemistry, and CSF were unremarkable. Serologic and CSF screening for VDRL, HIV, Lyme, VZV, CMV, and HSV were negative. CSF cultures grew no organisms. ANA, serum and CSF ACE, anti-TPO, ESR and CRP screening revealed only mild CRP elevation. Biopsy was initially deferred due to patient’s preference to avoid brain biopsy. Tolosa-Hunt syndrome was suspected, and the patient was given high-dose IV dexamethasone. After 3 days the eye pain resolved, but diplopia remained. He was discharged on a 2-week dexamethasone taper.
One month after dexamethasone completion, the patient reported minimal improvement. He underwent fine needle aspiration of the right pterygopalatine fossa, revealing atypical squa-mous cells and keratin pearls consistent with squamous cell carcinoma. Treatment with radiation and systemic chemotherapy was initiated.
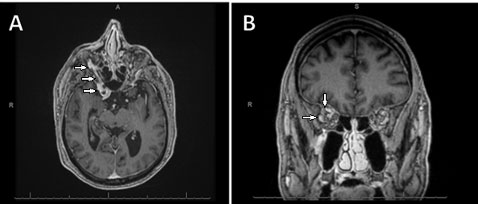
Figure 1. T1 weighted 3D MRI of the orbits demonstrating a contrast-enhancing soft tissue mass in the right cavernous sinus, extending into the right orbital apex, obliterating Meckel’s cave and ranging into the foramen ovale. A = axial view. B = coronal view.
Discussion
Tolosa-Hunt is a rare syndrome with symptoms of unilateral headache with ipsilateral ophthalmoplegia.1-2 The annual incidence is estimated at one case per million.3 MRI with contrast is highly sensitive for diagnosis. Glucocorticoids are considered the first-line treatment.4-5 Our patient appeared to meet the criteria for Tolosa-Hunt and was discharged on glucocorticoids (Figure 2).
Other causes of cranial neuropathy including malignancy, autoimmune or vascular disease must be eliminated to diagnose Tolosa-Hunt.6 Considering the cost-effectiveness of successful dexamethasone treatment, and the inherent risks of accessing the cavernous sinus, a shared decision was made to initiate dexamethasone before attempting the biopsy. However, other case reports have suggested prioritizing tissue biopsy before considering a diagnosis of Tolosa-Hunt.7
With failure of dexamethasone treatment, biopsy became necessary. Ultimately, he was found to have squamous cell carcinoma imitating Tolosa-Hunt. No other primary lesions were found, but the patient had a history of multiple skin cancers including a squamous cell carcinoma in 2004. Metastasis of skin cancer, particularly squamous cell carcinoma, may occur via perineural spread.7-9 It is important for physicians to recognize cranial neuropathies as a potential sign of perineural invasion in patients with a history of facial skin cancer. This case reinforces Tolosa-Hunt syndrome as a diagnosis of exclusion. Tissue biopsy is a necessary measure to rule out malignancy when differentiating an orbital mass.
Criteria for the diagnosis of Tolosa-Hunt Syndrome
All of the following criteria must be met:
1. Presence of granulomatous inflammation of cavernous sinus, superior orbital fissure, or orbit, seen on MRI or biopsy.
2. Unilateral palsies of one or more of cranial nerves III, IV, or VI.
3. Ipsilateral and unilateral headache which preceded the cranial neuropathy by two weeks or less.
4. Not better explained by another etiology.
Figure 2. Criteria for diagnosis of Tolosa-Hunt syndrome, as described by the Headache Classification Committee of the International Headache Society (IHS). All the above criteria must be met for diagnosis.
Author Information
Corresponding Author
* Rameez Zaman, BS
rzaman1@pennstatehealth.psu.edu
Author Contributions
All authors have given approval to the final version of the manuscript.
Funding Sources
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Disclosures
No authors have any disclosures or conflicts of interest at this time.
Acknowledgements
None.
References
1. Hunt, W. E., Meagher, J. N., LeFever, H. E., & Zeman, W. (1961). Painful ophthalmoplegia: its relation to indolent inflammation of the cavernous sinus. Neurology, 11(1), 56-56.
2. Tolosa, E. (1954). Periarteritic lesions of the carotid siphon with the clinical features of a carotid infraclinoidal aneu-rysm. Journal of Neurology, Neurosurgery, and Psychiatry, 17(4), 300.
3. Iaconetta, G., Stella, L., Esposito, M., & Cappabianca, P. (2005). Tolosa-Hunt syndrome extending in the cerebel-lopontine angle. Cephalalgia, 25(9), 746-750.
4. Jain, R., Sawhney, S., Koul, R. L., & Chand, P. (2008). Tolosa–Hunt syndrome: MRI appearances. Journal of Medical Imaging and Radiation Oncology, 52(5), 447-451.
5. Swerdlow, B. (1980). Tolosa‐hunt syndrome: A case with associated facial nerve palsy. Annals of Neurology: Official Journal of the American Neurological Association and the Child Neurology Society, 8(5), 542-543.
6. Headache Classification Committee of the International Headache Society (IHS). (2013). The international classifi-cation of headache disorders, (beta version). Cephalalgia, 33(9), 629-808.
7. Esmaeli, B., Ginsberg, L., Goepfert, H., & Deavers, M. (2000). Squamous cell carcinoma with perineural invasion present-ing as a Tolosa-Hunt-like syndrome: a potential pitfall in diagnosis. Ophthalmic Plastic & Reconstructive Surgery, 16(6), 450-452.
8. Koukkoulli, A., Koutroumanos, N., & Kidd, D. (2015). Perineural spread of cutaneous squamous cell carcinoma manifesting as ophthalmoplegia. Neuroophthalmology, 39(3), 144-146.
9. Nieto Enriquez, J., Medel Jiménez, R., & Huguet Redecilla, P. (2009). Undiagnosed squamous cell carcinoma of the forehead presenting as a Tolosa-Hunt syndrome. Orbit, 28(5), 290-292.