Learning Objectives
1. Evaluate the etiology and pathophysiology of oculopalatal tremor in the setting of hypertrophic olivary degeneration
2. Use the distinct physical exam findings to characterize oculopalatal tremor
3. Demonstrate the characteristic findings of hypertrophic olivary degeneration on MRI and list differential diagnosis associated with the imaging findings
Case Presentation
Case 1
Patient A is a 74-year-old gentleman who experienced a stroke in 2015 resulting in persistent bilateral vertical diplopia, dysphagia, decreased facial sensation in the left V3 distribution and right-sided weakness, with the lower extremity affected more. He presented in 2018 with new symptoms of difficulty reading and constant vertigo relieved only by closing both eyes. On exam, in addition to the deficits consistent with the old stroke, he had pendular nystagmus, and a facial tremor at the right corner of his lip that was the same frequency as his nystagmus. His uvula could not be visualized secondary to posterior oropharyngeal crowding. Notably there was intact cerebellar function without signs of ataxia or dysmetria. MRI Brain with contrast in 2019 showed evidence of a previous left medullary ischemic stroke, with olivary hypertrophy (Figure 1).
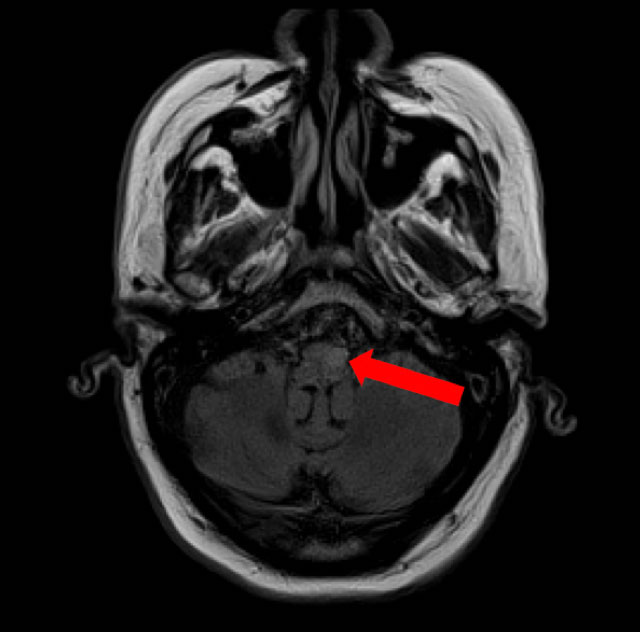
Figure 1. Axial T2/FLAIR MRI demonstrating left hypertrophic olivary degeneration (red arrow).
Case 2
Patient B is a 58-year-old woman who had a pontine hemorrhage due to cavernous malformation in 2017 (Figure 2A) that resulted in left sided weakness worse in the distal extremities. She also had diminished sensation only to pinprick on her left side, occasional vertigo and dysarthria secondary to true vocal cord paralysis resulting in hoarseness. She had multiple subsequent hemorrhages prior to treatment with gamma knife. She presented in 2018 with vertigo and gait ataxia. On exam she had a mild pendular nystagmus that was the same frequency as the associated palatal myoclonus, mild upper extremity dysmetria bilaterally and a wide-based ataxic gait. MRI brain imaging in 2018 showed signs of right hypertrophic olivary degeneration (Figure 2B).
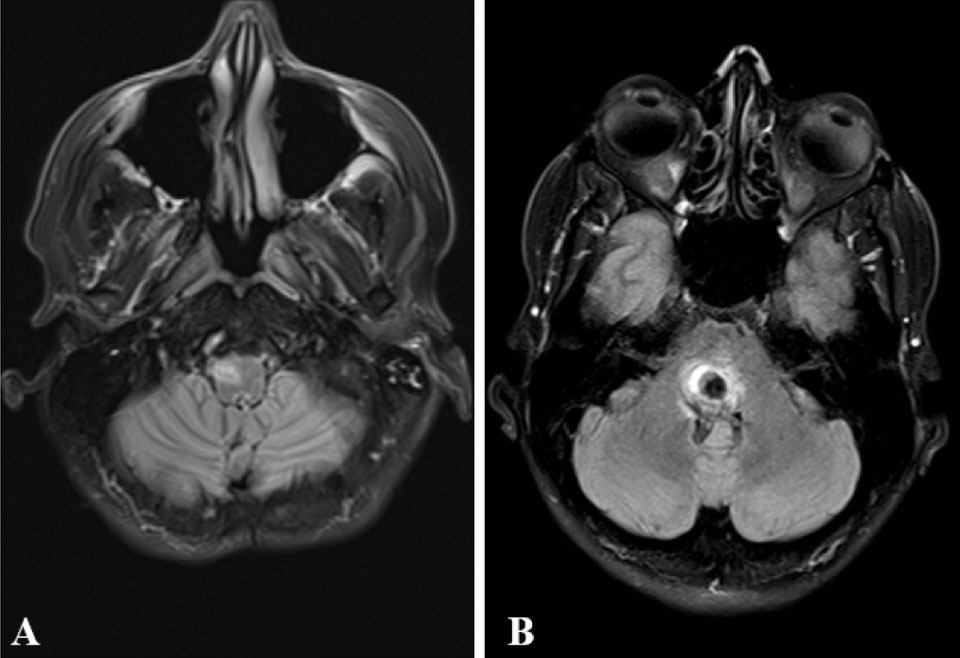
Figure 2. Axial T2/FLAIR MRI. A: MRI from August 2017 demonstrates subacute pontine hemorrhage (red arrow). B: MRI from December 2018 demonstrates right hypertrophic olivary degeneration (black arrow).
Discussion
Hypertrophic olivary degeneration (HOD) is a rare type of neuronal degeneration associated with the oculopalatal tremor (OPT) syndrome, which is most notable for a synchronous pendular nystagmus and palatal tremor.1,2 Involvement of other muscles developing from the branchial arches can also be seen.1 The palatal tremor, commonly bilateral and symmetric, is characterized by involuntary movements of the soft palate and pharynx as a result of rhythmic contraction of the levator veli palatini. The palatal movements are continuous, persist during sleep, and frequently occur at 1.5-3Hz.1 In addition to the palatal movements, 30% of sympto-matic patients present with a characteristic pendular nystagmus.1 The palatal tremor is often asymptomatic and usually does not cause trouble with speech or swallowing, however, patients may complain of hearing a clicking sound.1,3 The nystagmus is not directional, typically presenting with asymmetric vertical pendular oscillations of the eyes, with varied combinations of torsional and horizontal components, with a large mean amplitude, and high peak velocity.1 Patients typically complain of disturbing oscillopsia and decreased visual acuity related to the nystagmus.1,3
OPT results from damage to any part of the dentato-rubro-olivary pathway (DROP). Also known as the Guillain-Mollaret triangle, this is a neuroanatomical pathway involved in coordinating movement. This pathway consists of the ipsilateral red nucleus in the midbrain, the inferior olive in the medulla, and the contralateral dentate nucleus in the cerebellum.3 Many focal pathological processes are known to interrupt the pathway including ischemic injury, hemorrhage, demyelination, neoplasia, trauma, and surgery.4 Once the pathway becomes interrupted, the inferior olivary nucleus is no longer inhibited resulting in hypertrophy.3
Characteristics suggestive of HOD on MRI include high T2 signal intensity of the olivary nucleus , lack of contrast enhancement or diffusion restriction, and the presence of an inciting lesion in the ipsilateral brain stem or contralateral cerebellum.4 Increased T2 signal change can be seen about one month after insult to DROP3 with enlargement of the inferior olivary nucleus occurring four to six months later.4 Eventually, the enlargement of the inferior olivary nucleus resolves, but the T2 hyperintensity remains indefinitely.4 Therefore, the lack of enlargement does not exclude the diagnosis of HOD.4
Presence of an oculopalatal tremor is a rare exam finding that localizes to the olivary nucleus, however it is not specific to a single etiology. The rest of the clinical features, in addition to the associated radiologic findings, play a significant role in identification of a specific etiology. Both patients had an oculopalatal tremor as a result of hypertrophic olivary degeneration as determined by their physical exam and radiologic findings. However, patient A’s symptoms were a result of an ischemic medullary stroke, while patient B’s were from pontine hemorrhages and gamma knife treatment. These cases exemplify the various etiologies and help to further elucidate epidemiologic factors associated with this condition, thereby contributing to an increased understanding of this rare phenomenon.
There is no definitive treatment available for symptoms. Medications such as gabapentin, memantine, clonazepam, baclofen have been used with variable response.1
Author Information
Corresponding Author
* April Henry, BS
ahenry2@pennstatehealth.psu.edu, 904-534-2392
Author Contributions
All author(s) have given approval to the final version of the manuscript.
Funding Sources
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Disclosures
No author(s) have any disclosures or conflicts of interest at this time.
Acknowledgements
None.
References
1. Tilikete, C., & Desestret, V. (2017). Hypertrophic olivary degeneration and palatal or oculopalatal tremor. Frontiers in Neurology, 8, 302.
2. Kattah, J. C., Elble, R. J., De Santo, J., & Shaikh, A. G. (2020). Oculopalatal tremor following sequential medullary infarcts that did not cause hypertrophic olivary degeneration. Cerebellum & Ataxias, 7(1), 1-5.
3. Murdoch, S., Shah, P., & Jampana, R. (2016). The Guillain-Mollaret triangle in action. Practical Neurology, 16(3), 243-246.
4 Eetvelde, M. L., Backaert, T., Favoreel, N., Geerts, B., Sommeling, C., Hemelsoet, D., & Dekeyzer, S. (2016). Imaging features of hypertrophic olivary degeneration. Journal of the Belgian Society of Radiology, 100(1).