Disclaimer
The Pennsylvania State University is not a NIOSH testing facility. Although we attempted to follow best practices, due to the limitations discussed below and the urgent need for data, modifications were made to normal testing procedure. This test data is provided for informational, educational, and research purposes only. We encourage independent validation with proper ASTM and NIOSH testing procedure before considering the use any of these materials in a mask or respirator device.
Introduction
Due to COVID-19, there is currently an international shortage of many important types of personal protective equipment (PPE) needed by healthcare workers caring for COVID-19 patients, including both N95 respirators and medical face masks.1 As a result, there is a pressing need for alternatives to commercially-made masks, both for healthcare professionals and the public, to protect themselves from exposure to COVID-19. While prior studies have evaluated the potential of household materials for use in masks,2-6 an explosion of online “DIY mask” instructions using novel materials, as well as conflicting data from widely publicized but yet-to-be peer reviewed research,7-9 and public warnings from some of the manufacturers of these “recommended materials” cautioning against off-label use,10,11 indicate the need for further study. We hypothesize that many of the materials being utilized in improvised masks may provide poor filtration efficiency compared to N95 respirators or medical masks.
Face Masks vs. N95 Respirators
There are three types of masks widely used in healthcare: procedural masks, surgical masks, and surgical N95 respirators. While procedure and surgical masks often share similar construction, procedure masks are designed for short-term use and are usually secured with ear loops, whereas surgical masks are designed to be worn for extended periods of time and are usually secured with ties. Both surgical and procedure masks are often collectively referred to as “medical masks” or “simple face masks.” They are produced according to American Society of Testing and Materials (ASTM) standards and are rated based on fluid resistance, bacterial and particle filtration efficiency, breathability (pressure drop through the mask), and flame resistance.12 The masks often contain multiple filter layers as well as additional components to help them mold to the face.13
Standard N95 respirators are rated by the National Institute of Occupational Safety and Health (NIOSH) and designed to provide ≥ 95% filtration efficiency of 0.3 micron of non-oily particles.14 A subset of N95 respirators, the surgical N95 respirator, is also approved by the FDA as a surgical mask and provides fluid resistance.15 A summary of the different standards used to rate protective masks and respirators is shown in Table 1.
Table 1. Industry Standards for Face Masks
|
ASTM 1 |
ASTM 2 |
ASTM 3 |
NIOSH N95 |
Surgical N95 |
|
|
Fluid Resistance |
80 mmHg |
120 mmHg |
160 mmHg |
None |
120 mmHg-160 mmHg |
|
Bacterial Efficiency |
≥ 95% |
≥ 98% |
≥ 98% |
||
|
Particulate Efficiency |
≥ 95% @ 0.1 micron |
≥ 98% @ 0.1 micron |
≥ 98% @ 0.1 micron |
≥ 95% @ 0.3 micron |
≥ 95% @ 0.3 micron |
|
DeltaP (Breathability) |
< 4.0 mm |
< 5.0 mm |
< 5.0 mm |
||
|
Flame Spread Class |
1 |
1 |
1 |
Characterization of the SARS-CoV-2 virus (COVID-19) was published in February 2020, in which electron micrographs of SARS-CoV-2 virus showed the extracellular inclusion bodies were “spherical with some pleomorphism” and ranged in diameter from 60 to 40 nm while viral particles spiked at 9 nm to 12 nm.16 Although these particles are smaller than 0.3 µm, NIOSH considers 0.3 µm to be the “most penetrating aerosol size” and utilizes them in its filtration certification tests in an effort to simulate the “worst-case” a mask would likely encounter.14 This is supported in a NASA analysis of HEPA filters in which they explain how ultrafine particulate matter (defined in the analysis as <0.1 µm) is predominantly filtered via diffusion whereas fine particles (1 µm < 2.5 µm) are predominantly subjected to interception and impaction with the filter. Submicron particulate matter (0.1 µm < 1 µm) falls between these ranges, allowing it to more easily penetrate filter material.17
According to the Centers for Disease Control and Prevention (CDC), COVID-19 is primarily spread by respiratory droplets (defined as >5 µm), and it is uncertain if droplet nuclei (defined as ≤5 µm) are viable vectors for transmission.18,19 Even if COVID-19 is able to spread as an aerosol, studies show that most infectious respiratory particles from humans exist as droplet nuclei ranging in diameter from 0.5 µm to 5 µm. Thus, it is unlikely that a mask would need to filter a viral particle in isolation, making 0.3 µm an acceptable measure for filtration efficiency.20 At the time of paper submission, the current CDC guidance for caring for an unmasked COVID-19 patient is an N95 respirator.21

Figure 1: Settings for measurements. |

Figure 2. Measuring background particles in room. |

Figure 3. Measuring MERV 15 material capacity in room at 0.1 CFM. |
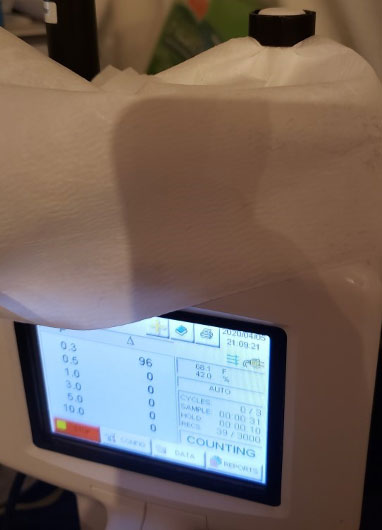
Figure 4. Measuring MERV 15 material capacity in room at 0.1 CFM. |
Methods
N95 respirators are certified by NIOSH using the Determination of Particulate Filter Efficiency Level For N95 Series Filters Against Solid Particulates For Non-Powered, Air-Purifying Respirators Standard Testing Procedure (STP)22 while medical masks must meet ASTM F2100-19 Standard Specification for Performance of Materials Used in Medical Face Masks.23
To conduct this study, we first attempted to acquire the standard NIOSH testing apparatus. However, due to the COVID-19 pandemic, we were unable to procure the apparatus or similar aerosol generation equipment for use according to the NIOSH and ASTM test methods. Submitting material to NIOSH for testing was also not possible due to the extended turnaround time.
With the need for rapid evaluation of masks and filter media, it was necessary to establish an alternative testing procedure. The standard test methods use a monodispersed aerosol with a particle size of about 180 nm, but we did not have the necessary equipment available onsite. We instead used polydispersed particles from the air and a Lighthouse 3016 Particle Counter that was able to separate particles by size and count them. The particle counter was calibrated by Lighthouse Worldwide Solutions, a National Institute of Standards and Technology (NIST) traceable lab. This procedure utilized particles in the room air as a baseline (similar to what a virus might attach to) and a particle counter to count the number of particles in the room compared to the number that successfully passed through the filter media or mask. Since no human subjects were utilized, IRB approval was not required.
We identified candidate materials for evaluation after reviewing media reports regarding what other health systems and “DIYers” were using in their improvised masks. The final materials were selected for testing based on local availability to our affiliated academic medical center in the event that they elected to begin mask production.
Cotton T-shirts had been previously been identified as potential improvised mask material and are currently one of the fabrics listed by the CDC in their instructions for making cloth face coverings.2,24 Minimum Efficiency Reporting Values (MERV) 13 and higher furnace filters have been widely reported in the media as good mask filter material as they are designed to filter out allergens and bacteria without impeding airflow.25,26
Meltblown fabric was chosen to test as it is used as the filter in most N95 respirators and simple face masks and can be purchased separately from manufacturers.13 Surgical sterilization wrap was reportedly used to make improvised masks for at least one health system and is a waste product for most hospitals, so it is in ample supply.27 It is made from two layers of thermally sealed non-woven polypropylene and comes in different grades, of which we tested the heaviest. Not only is it designed to act as a microbial barrier, but it can be autoclaved, so it would likely withstand various decontamination methods. Both paper towels and non-woven polypropylene blue shop towels were also selected due to media reports of their high filtration efficiencies and wide availability.8,28
Lastly, due to our hospital’s proximity to a local wool hat manufacturer, we tested various types of wool felt which underwent different manufacturing processes such as dusting, washing, or dying, as well as a proprietary treatment which makes the wool water repellant and helps it retain its shape. The wool felt samples were also shrunk by different amounts, meaning they were mechanically processed so that the fibers reoriented and became more condensed. Shrink is recorded as a percentage of the fabric’s original dimensions. Some samples were tested in multiple layers. Commercially available masks including a brand-name N95 respirator, KN95 respirator, and cleanroom mask (similar to a surgical mask) were tested so they could be compared against the other materials tested.
Setup
Detector Model:
• Lighthouse 3016
Detector Settings:
• Units: ft^3
• Acquisition time: 60 s
• Internal pump flow rate: 0.1 CFM for handheld unit
• Funnel Area: 95 mm2
• Measures particles of size: 0.3 µm, 0.5 µm, 1 µm, 3 µm, 5 µm, 10 µm
• Prior to set of runs use PALL zero filter to check background counts (should be <10)
• All counts should be of Cumulative type
Procedure
The particle counter was configured with settings as shown in Figure 1. A background sample of particles was collected using the setup pictured in Figure 2, with the test funnel directly connected to the handheld particle counter. Each measurement was repeated 3 times before and 3 times after the test sample for the control (a total of 6 times) and 3 times for each of the test materials.
Steps
1. Obtain data for the control tests by recording 3 consecutive measurements of the number of particles in the room.
2. Apply the test filter over the mouth of the funnel and secure tightly with a rubber band, pipe clamp, or nut as shown in Figure 3 and Figure 4. Obtain 3 measurements of the number of particles passing through the filter material. Up to 3 different filter media can be measured before proceeding to Step 3.
3. Repeat the control by measuring the number of particles in the room 3 consecutive times. For best results, the time between Step 1 and Step 3 should be minimized.
4. Calculate the average number of particles recorded during the control tests.
5. Calculate the average number of particles recorded during the filter tests.
6. Calculate the particle filtration efficiency for each particle size using the following formula:
a. (Room Average Counts - Filter Average Counts) / Room Average Counts
b. If the material sheds (data shows more particles recorded with the test material than the control), an efficiency of zero is assigned
Results
The filtration efficiencies for particles ranging from 0.3 µm to 10.0 µm were obtained and have been color-coded based on the filtration efficiency thresholds outlined in Table 2. The results are shown in Tables 3, 4, and 5. The ply indicates the number of layers of the product used in the test, not the number of plys the product is made from. The test setup was validated with a 0.2 µm laboratory filter to ensure the testing apparatus was not shedding any particles that could alter results.
Discussion
As expected, the commercially produced N95 respirator exceeded the 95% filtration efficiency criteria and performed better than the medical mask. The MERV 15 filter material also met the 95% filtration efficiency at 0.3 µm at 2-ply, while the meltblown fabric required at least 4-ply to meet this standard. However, none of the remaining samples we tested met the filtration efficiency of either a medical mask or N95 respirator, indicating that our hypothesis was correct and many of the “DIY masks” were using inferior material. This was consistent with much of the prior literature which found that many household materials had low filtration efficiencies2,5 while others had a high pressure drop2,4,6 that would potentially make the material difficult to breathe through.
Although they did not match the filtration efficiency of the N95 respirator or cleanroom mask, we believe that some of the materials we tested merit further exploration and possible consideration as mask materials. When layered in multiple plys, the MERV 13 filter, sterilization wrap, and paper towels, as well as some of the wool felt samples in 1-ply, had superior filtration efficiency to the current CDC recommendation of a cotton T-shirt for the public to utilize in homemade masks.24 Not only could these materials, should their parameters meet the other considerations for use in a mask, be beneficial for public “DIY masks,” but they could potentially be used as a layer in a composite mask made with multiple materials to achieve a higher filtration efficiency. Similar studies have also found higher filtration efficiencies when different types of materials were layered together3,4 or when household materials were given a static charge.6
While there is significant research interest in alternative materials to use in masks, the differences in test methods including the area of the sample tested, how the testing apparatus secures the sample, particle size tested, flowrate, and material types tested makes it difficult to compare results. Additionally, even when studies utilize a similar test method, the wide variation of products such as paper towels or cotton T-shirts means that even studies that appear to test the same material may actually be testing samples with completely different properties.
Compared to previous data on the filtration efficiency of 2 layers of cotton T-shirt at 1 µm, we obtained an approximately 20% lower filtration efficiency than one study whereas other studies investigating cotton T-shirts used only a single layer of material and found lower filtration efficiencies than we obtained.2,5,6 However, due to potential differences in the shirt materials, the small sample size of our test, and the wide variation in results in one of the studies, this result is not unexpected and only helps illustrate the need for more consistent data.6
Although the wool felt and MERV 13 filter were able to provide greater than 60% filtration efficiency with a single ply, the sterilization wrap and paper towels required multiple plys to provide similar levels of filtration. Not only could this result in a significant pressure drop across the filter which would make the mask difficult to breathe through, but many online tutorials recommending these materials do not indicate the need for multiple layers. Therefore, many “DIY masks” using these materials may provide less filtration, and thus be less protective, than the wearer believes.
In addition to concerns regarding the pressure drop with multiple layers, the availability and durability of these materials are important considerations. While paper towels are inexpensive and widely available, it is unlikely that they would be able to be safely disinfected and reused, meaning that they would only be viable in a mask designed for a single use for a short period of time. Additionally, other research determined that paper towels have a much lower filtration efficiency than our study found. Similar to our experience testing cotton, it is unclear if they used the same brand or number of plys as we tested, further illustrating both the difficulty in comparing data between different studies as well as the challenge a layperson encounters when attempting to follow recommendations when selecting material to use in a DIY mask.6
Although the MERV 13 filter is designed to allow for easy airflow so that breathability is less likely to be an issue with use in multiple layers than some of the other materials tested, there are many limitations to its use in a mask. Many of these filters are made from fiberglass, which could be dangerous if the filter shed particles that were inhaled. These filters would thus require additional material to protect the user. The MERV 13 samples tested in this study were electrostatic filters which do not contain fiberglass, but rely on an electrostatic charge to capture particles. These filters can be inactivated when they become wet, so any mask would require a fluid barrier to protect the filter and likely could not be laundered.
Though it did not perform as well as the MERV-rated filters, the surgical sterilization wrap in multiple plys performed better than the paper towels and wool. Not only is sterilization wrap readily available, as it is currently a waste product at most hospitals, but its ability to be autoclaved and disinfected makes its reuse viable. Although it would not offer as high a filtration efficiency as a manufactured mask or some of the other materials tested, its availability, low cost, durability, and ability to be used as the mask itself instead of just a filter insert could make it a viable option for mask use in low risk settings.
The 100% wool felt had wide variations in filtration efficiencies among the different samples that were tested. While it was unsurprising that the 30% wool shrink greatly underperformed the 65% and 68% shrink samples that had more tightly compressed fibers, the differing finishing processes used on the different 68% shrink dyed wool samples improved the filtration efficiency over the un-dyed samples to different degrees. Additionally, some samples showed a large decrease in filtration efficiency of larger particles compared to the filtration efficiency of the smaller particles. It is suspected that these samples may have shed particles during testing and contaminated the results. As such, further processing and re-testing of the samples should be performed before utilization of these samples as mask material.
Limitations
Due to limitations of the test setup, we tested the filter samples using a flow rate of 0.1 CFM, or approximately 28 LPM over the sample area of 95 mm. While this is lower than the NIOSH test protocol which calls for 85 LPM, because this flow rate was applied over the smaller sample area as opposed to the entire mask, it likely produced a higher effective flow rate than the NIOSH testing protocol. While a higher flow rate should reduce filter efficiency, as particles have a higher velocity and less time to be captured by an electrostatic charge, it may also change how some of the particles interacted with the filter material via impaction. Therefore, although we believe our results were produced under more strenuous test conditions than the NIOSH protocol, any material which will be used in an N95 respirator should be tested under the NIOSH conditions.
Additionally, the same samples were tested only 3 times. Therefore, additional testing of different samples of the same material and under different use conditions are necessary to ensure that the materials are uniform in quality, will not be affected by factors such as humidity, and will provide reliable protection if used in mask construction. Although the authors inspected the data to ensure there were no obvious outliers in any of the results, detailed statistical calculations were not undertaken due to the preliminary nature of this research and will need to be performed after more samples are tested.
While this study addressed the filtration efficiency of these materials, there are additional material properties that will affect the viability of their use in a mask. Further testing of filter parameters such as pressure drop, durability, fluid resistance, ability to withstand washing or disinfection, and safety are needed before any of these materials should be used in a mask.
Conclusion
While some of the filter materials tested had a high enough filtration efficiency to meet NIOSH N95 requirements, many of the nontraditional filter materials tested were inferior to commercially manufactured masks. However, when used in multiple plys, some did provide superior filtration to the materials currently recommended to the public for mask use. Therefore, they may be beneficial for use in homemade masks for the public or as a layer in a composite mask for healthcare workers.
Author Information
Corresponding Author
*Daniel Berger, B.S.
dberger1@pennstatehealth.psu.edu
Author Contributions
All authors have given approval to the final version of the manuscript.
Funding Sources
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Disclosures
No authors have any disclosures or conflicts of interest at this time.
Acknowledgements
The authors would like to thank the team members of Penn State University’s Manufacturing and Sterilization for COVID-19 (MASC) Initiative for their assistance in the provision of test samples, technical expertise, and instrumentation. They would also like to thank Bollman Hat Company for generously donating the wool felt material samples.
Color legend for Tables 3, 4 and 5
|
0-9.9% |
10-19.9% |
20-29.9% |
30-39.9% |
40-49.9% |
50-59.9% |
60-69.9% |
70-79.9% |
80-89.9% |
90-94.9% |
95-99.9% |
100% |
Table 3. Filtration efficiencies for a brand-name N95 respirator, cleanroom mask, KN95 respirator, selected furnace filters, and meltblown fabric. A 0.2 μm laboratory filter was tested to validate the testing apparatus.
|
Sample Label |
% Efficiency |
% Efficiency |
% Efficiency |
% Efficiency |
% Efficiency |
% Efficiency |
|
0.2 μm Labratory Filter |
100.0 |
100.0 |
100.0 |
100.0 |
100.0 |
100.0 |
|
N95 Respirator |
98.0 |
99.5 |
99.8 |
100.0 |
100.0 |
100.0 |
|
Cleanroom Mask |
86.3 |
97.3 |
98.8 |
99.6 |
100.0 |
100.0 |
|
KN95 Respirator |
83.9 |
96.1 |
99.0 |
100.0 |
100.0 |
100.0 |
|
MERV 13 Electrostatic Filter |
61.8 |
81.7 |
90.2 |
95.7 |
97.0 |
100.0 |
|
MERV 13 Electrostatic Filter 2-Ply |
83.2 |
95.1 |
97.9 |
100.0 |
100.0 |
100.0 |
|
MERV 13 Bag Filter 2-Ply |
95.1 |
99.6 |
100.0 |
100.0 |
100.0 |
100.0 |
|
Meltblown 1-Ply |
74.9 |
93.8 |
99.4 |
100.0 |
100.0 |
100.0 |
|
Meltblown 2-Ply |
78.6 |
97.0 |
99.8 |
100.0 |
100.0 |
100.0 |
|
Meltblown 3-Ply |
82.7 |
98.0 |
100.0 |
100.0 |
100.0 |
100.0 |
|
Meltblown 4-Ply |
95.5 |
99.7 |
100.0 |
100.0 |
100.0 |
100.0 |
|
Meltblown 5-Ply |
98.7 |
100.0 |
100.0 |
100.0 |
100.0 |
100.0 |
|
Meltblown 6-Ply |
99.2 |
100.0 |
100.0 |
100.0 |
100.0 |
100.0 |
Table 4. Filtration efficiencies for 100% cotton fabric and a selection of 100% wool felts (WF) of different shrinks (percentages) that include both dyed (D) and un-dyed (UD) as well as various finishing treatments.
|
Sample Label |
% Efficiency |
% Efficiency |
% Efficiency |
% Efficiency |
% Efficiency |
% Efficiency |
|
100% Cotton 2-Ply |
28.7 |
48.9 |
57.7 |
65.4 |
70.1 |
66.7 |
|
WF, UD 30% Shrink |
19.9 |
48.1 |
83.6 |
92.0 |
85.7 |
22.2 |
|
WF, UD 65% Shrink |
36.8 |
77.6 |
98.3 |
100.0 |
100.0 |
100.0 |
|
WF, D, 68% Shrink, Treatment 1 |
45.5 |
87.1 |
98.7 |
99.2 |
98.4 |
95.0 |
|
WF, D 68% Shrink, Treatment 2 |
62.2 |
92.6 |
98.9 |
98.6 |
97.5 |
89.1 |
|
WF, D 68% Shrink, Treatment 3 |
55.8 |
85.4 |
90.1 |
83.8 |
74.4 |
19.6 |
Table 5. Filtration efficiencies for brand-name paper hand towels, brand-name polypropylene shop towels, and brand name sterilization wrap.
|
Sample Label |
% Efficiency |
% Efficiency |
% Efficiency |
% Efficiency |
% Efficiency |
% Efficiency |
|
Brand-Name Hand Towel 3-Ply |
49.1 |
81.2 |
98.3 |
100.0 |
100.0 |
100.0 |
|
Brand-Name Hand Towel 4-Ply |
62.6 |
90.7 |
99.7 |
100.0 |
100.0 |
100.0 |
|
Brand-Name Hand Towel 5-Ply |
68.5 |
93.8 |
99.7 |
100.0 |
100.0 |
100.0 |
|
Brand-Name Shop Towel 2-Ply |
19.8 |
48.4 |
76.8 |
85.1 |
82.1 |
87.0 |
|
Sterilization Wrap 1-Ply |
42.4 |
70.8 |
83.6 |
87.8 |
89.6 |
100.0 |
|
Sterilization Wrap 2-Ply |
75.5 |
94.7 |
97.9 |
98.6 |
98.5 |
100.0 |
|
Sterilization Wrap 3-Ply |
79.9 |
96.2 |
98.8 |
99.3 |
100.0 |
100.0 |
References
1. World Health Organization. (2020). Shortage of personal protective equipment endangering health workers worldwide. World Health Organization. Retrieved from: https://www.who.int/news-room/detail/03-03-2020-shortage-of-personal-protective-equipment-endangering-health-workers-worldwide
2. Davies, A., Thompson, K. A., Giri, K., Kafatos, G., Walker, J., & Bennett, A. (2013). Testing the efficacy of homemade masks: would they protect in an influenza pandemic? Disaster medicine and public health preparedness, 7(4), 413–418. https://doi.org/10.1017/dmp.2013.43
3. Konda, A., Prakash, A., Moss, G. A., Schmoldt, M., Grant, G. D., & Guha, S. (2020). Aerosol Filtration Efficiency of Common Fabrics Used in Respiratory Cloth Masks. ACS nano, 14(5), 6339–6347. https://doi.org/10.1021/acsnano.0c03252
4. Lustig, S. R., Biswakarma, J., Rana, D., Tilford, S. H., Hu, W., Su, M., & Rosenblatt, M. S. (2020). Effectiveness of Common Fabrics to Block Aqueous Aerosols of Virus-like Nanoparticles. ACS nano, 14(6), 7651–7658. https://doi.org/10.1021/acsnano.0c03972
5. Rengasamy S, Eimer B, Shaffer RE. Simple respiratory protection--evaluation of the filtration performance of cloth masks and common fabric materials against 20-1000 nm size particles. Ann Occup Hyg. 2010;54(7):789-798. doi:10.1093/annhyg/meq044
6. Zhao, M., Liao, L., Xiao, W., Yu, X., Wang, H., Wang, Q., Lin, Y. L., Kilinc-Balci, F. S., Price, A., Chu, L., Chu, M. C., Chu, S., & Cui, Y. (2020). Household Materials Selection for Homemade Cloth Face Coverings and Their Filtration Efficiency Enhancement with Triboelectric Charging. Nano letters, acs.nanolett.0c02211. Advance online publication. https://doi.org/10.1021/acs.nanolett.0c02211
7. Careaga, Andrew. (2020). Environmental engineers study fabrics, materials for face covers. Retrieved from: https://news.mst.edu/2020/04/environmental-engineers-study-fabrics-materials-for-face-covers/
8. Robertson, Paddy. (2020). The Ultimate Guide to Homemade Face Masks for Coronavirus. Retrieved from: https://smartairfilters.com/en/blog/best-diy-coronavirus-homemade-mask-material-covid/
9. Wake Forest Baptist Health. (2020). Testing Shows Type of Cloth Used in Homemade Masks Makes a Difference, Doctors Say. Retrieved from: https://newsroom.wakehealth.edu/News-Releases/2020/04/Testing-Shows-Type-of-Cloth-Used-in-Homemade-Masks-Makes-a-Difference
10 3M. (2020). Coronavirus and Important Things to Know About Airborne Particles. Retrieved from: https://www.filtrete.com/3M/en_US/filtrete/home-tips/full-story/~/coronavirus-and-important-things-to-know-about-airborne-particles/?storyid=d69e7735-c02c-46d2-9c8a-ae23372934ac
11. O&M Halyard. (2020). Can I Use Halyard Sterilization Wrap for DIY Masks?. Retrieved from: https://www.halyardhealth.com/covid-19/diy-masks.aspx
12. Crosstex International. (2014). The right mask for the right team! MaskEnomics: The Crosstex guide to face mask selection and use. [Pamphlet]. Crosstex International.
13. Henneberry, Brittany. (n.d.) How Surgical Masks are Made, Retrieved from: https://www.thomasnet.com/articles/other/how-surgical-masks-are-made/#_How_are_Surgical
14. The National Institute for Occupational Safety and Health. (2014). NIOSH Guide to the Selection and Use of Particulate Respirators, Retrieved from: https://www.cdc.gov/niosh/docs/96-101/default.html
15. 3M. (2020). Surgical N95 vs. Standard N95 – Which to Consider? Rev. 2
16. [Technical Bulletin]. St. Paul, MN: 3M Personal Safety Division.
17. Zhu, Na, et al. (2019). A Novel Coronavirus from Patients with Pneumonia in China, New England Journal of Medicine, vol. 382, no. 8, 2020, pp. 727–733., 2019. doi:10.1056/nejmoa2001017
18. Perry, J.L., Agui, J.H., Vijayakumar, R. (2016). Submicron and Nanoparticulate Matter Removal by HEPA-Rated Media Filters and Packed Beds of Granular Materials. NASA STI, 2016. https://ntrs.nasa.gov/archive/nasa/casi.ntrs.nasa.gov/20170005166.pdf
19. Centers for Disease Control and Prevention. (2020). Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings. Retrieved from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html
20. Atkinson J, Chartier Y, Pessoa-Silva CL, et al., editors. (2009). Natural Ventilation for Infection Control in Health-Care Settings: Annex C, Respiratory Droplets. World Health Organization, 2009, https://www.ncbi.nlm.nih.gov/books/NBK143281
21. Fernstrom, A., Goldblatt, M. (2013). Aerobiology and its role in the transmission of infectious diseases. Journal of pathogens, 2013, 493960. https://doi.org/10.1155/2013/493960
22. Centers for Disease Control and Prevention. (2020). Strategies for Optimizing the Supply of N95 Respirators. Retrieved from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/respirators-strategy/index.html
23. The National Institute for Occupational Safety and Health National Personal Protective Technology Laboratory. (2019). Determination of particulate filter efficiency level for N95 series filters against solid particulates for non-powered, air-purifying respirators standard testing procedure (STP). Retrieved from: https://www.cdc.gov/niosh/npptl/stps/pdfs/TEB-APR-STP-0059-508.pdf
24. ASTM International. (2019). Standard Specification for Performance of Materials Used in Medical Face Masks, ASTM International, West Conshohocken, PA, 2019, http://www.astm.org/cgi-bin/resolver.cgi?F2100-19e1
25. Centers for Disease Control and Prevention. (2020). Use of Cloth Face Coverings to Help Slow the Spread of COVID-19. Retrieved from: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/diy-cloth-face-coverings.html
26. Dunning, Savana. (2020). Texas A&M researchers develop DIY respirators similar to N95s. Retrieved from: https://www.expressnews.com/news/health/article/Texas-A-M-researchers-develop-DIY-respirators-15169122.php
27. Simmons, Karie. (2020). Seamstresses step up to sew masks amid shortage. Retrieved from: https://thecharlotteweekly.com/news/2020/03/seamstresses-step-up-to-sew-masks-amid-shortage
28. Buletti, Leah. (2020). UF Health anesthesiology team devises respirator mask made from existing hospital materials. Retrieved from: https://ufhealth.org/news/2020/uf-health-anesthesiology-team-devises-respirator-mask-made-existing-hospital-materials
29. Bort, Julie. (2020, April 2). Using blue shop towels in homemade face masks can filter particles 2x to 3x better than cotton, 3 clothing designers discover after testing dozens of fabrics. Business Insider. Retrieved from: https://www.businessinsider.com/homemade-mask-using-hydro-knit-shop-towel-filters-better-2020-4