Background
Traditionally, neurology has been a field in which few medical students demonstrate a strong interest, which has been reflected in the residency match trends and data from graduating medical students. A study conducted in 2019, which analyzed allopathic graduate data from the AAMC Graduation Questionnaire (GQ), demonstrated that of almost fifty-two thousand students, only 1,456 or 2.8% were planning to go into neurology after graduation1. This pattern is concerning, as the burden of neurological disease increases while the neurological workforce remains stagnant. In fact, the deficit in the adult neurology workforce is estimated to increase by 19% by 2025, with a similar trend seen with child neurology1,2. Studies demonstrate that the reasons for this lack of interest and pursuit of neurological fields is linked to the concept of “neurophobia”, a term first introduced by Dr. Ralph F. Jozefowicz. He defined this phenomenon as “a fear of the neural sciences and clinical neurology that is due to the students’ inability to apply their knowledge of basic sciences to clinical situations3. Neurology is often regarded as one of the more difficult and comprehensive specialties, where students, residents, and practitioners are less confident than when dealing with other conditions4,5. Some factors that have been thought to contribute to neurophobia are complex neuroanatomy, insufficient teaching, lack of exposure, and a misconception that neurological sciences are innately hard and complicated6,7.Furthermore, medical students typically lack early and significant exposure to neurology. Neurology is not a universally required clinical clerkships at United States medical schools. In 2015, it was reported that only 56% of medical schools required any neurology clerkship. Furthermore, it was found that medical schools with required neurology clerkship had consistently high neurology match rates8. This may suggest that clinical exposure plays an important role in fostering neurology interest. However, other contributing factors are still yet to be elucidated.
Our objective was to elucidate whether there are factors beyond a required neurology clerkship that affect medical student interest in neurology, and how neurology curricula may impact this interest. We postulated that PSCOM would either meet or outperform the national average of medical students matching in neurology due to early exposure to clinical neurology and the presence of a required neurology clerkship.
Methods
We conducted two surveys; Survey 1 was distributed to a small group of students and Survey 2 was distributed to the student body of PSCOM. The goal of these surveys was to investigate student perception, pre-clinical exposure and comfort level with the field of neurology, as well as their impression of the neurology curriculum at PSCOM (Appendix A). Both surveys were developed by three of the authors. All survey respondents were recruited voluntarily and responses were anonymous. Survey 1 investigated student perception of their neurology exposure and the field, which was conducted in 2016 and structured as a combination of 5- and 4- point Likert scales with several dichotomous answers. It included one neurology faculty member’s mentees, serving as a means to gain a baseline understanding of student perceptions and interests. This survey was sent via email to one of the investigators’ mentees (21 total) and had 19 respondents. Survey 2 which investigated students’ perception of the quality of the neurology curriculum and their level of comfort in neurology, was conducted in 2017. This survey was structured as a combination of questions including a 4-point Likert scale, dichotomous answers, and one free response question. This survey was distributed via email to the entire PSCOM medical student body (600 potential respondents) from all years of training and had 175 respondents. Student interest in neurology was measured by residency match trends. We utilized publicly available neurology match results (adult and child M.D. neurology) from PSCOM were compared to data across the United States from 2011 to 20209,10. All statistical analyses of these populations were performed in Microsoft Excel including a 2-population Z-test with a statistical significance level of 0.05. As only publicly available and de-identified information was used, Institutional Review Board (IRB) approval was exempt.
Results
Survey 1 investigated student perception and comfort level with the field of neurology, a quantitative survey was conducted; this survey received 19 responses (90.4% of 21 potential; 5 M1, 4 M2, 6 M3 and 4 M4), however, some respondents did not complete all questions. This survey demonstrated that 64% (9/14) of respondents felt that they received adequate teaching in neuroscience, feeling either “average” or “very comfortable” performing the neurologic exam. Furthermore, 42% (8/19) of respondents considered neurology as a specialty. Respondents in the free response section reported that they largely felt that lectures, problem-based learning sessions, and Neurology Day (an event where patients with neurological disease teach students about their conditions) were the most helpful in aiding in their understanding of neurology. While the majority of students felt the preclinical years integrated clinical neurology (86.7%, 6/7) respondents from Survey 1), most reported less than (36%, 63/175) satisfactory or no (30%, 53/175) neurology exposure.
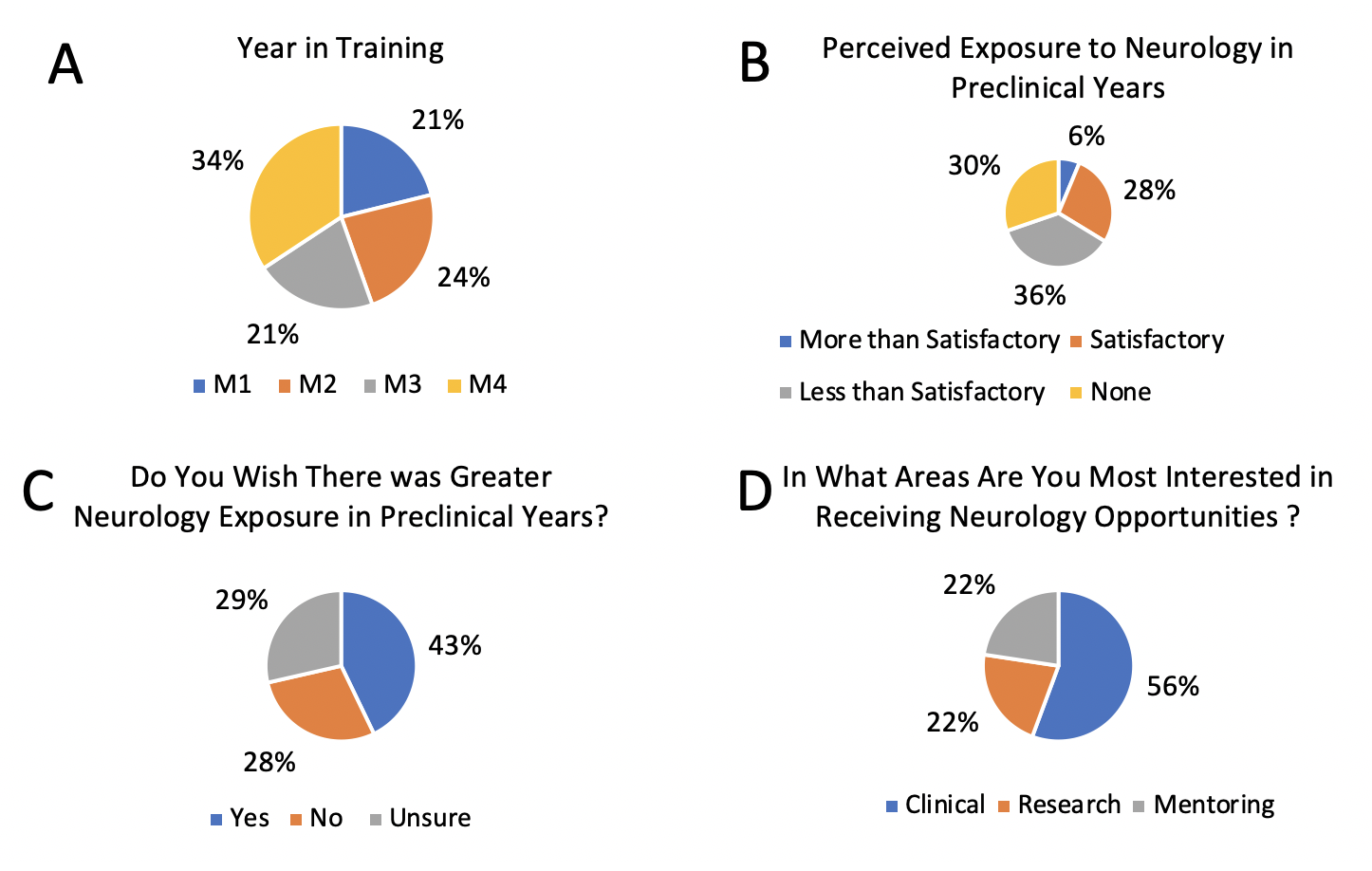
To further assess students’ satisfaction with the extent of exposure to neurology in preclinical years, a follow-up survey was conducted. This survey included questions that sought to explore whether they wished they had more exposure and whether they wished they had more opportunities in research, clinical areas, and mentoring. The small sample size of Survey 1 limits its generalizability, and was meant to be an initial screen of the perceptions of neurology at PSCOM. In order to gain a more comprehensive understanding of the student population at PSCOM regarding neurology interest Survey 2 was conducted. Among 175 respondents from all training years (29.2% of 600 potential) (Fig. 1A), the responses to perceived exposure to neurology in preclinical years (prior to the neurology block) were 30.3% (53/175) “none”, 36% (63/175) “less than satisfactory”, 27.4% (48/175) “satisfactory”, and 6.3% (11/175) “more than satisfactory” (Fig. 1B). First and second year medical students (M1-2s) reported “less than satisfactory” and “none” (41/78, 52%; 30/78, 38%) to a greater degree than M3-4s (22/97, 23%; 23/97,24%), who reported “satisfactory” predominantly (43/97, 44%). A majority of respondents wished for more opportunities to gain exposure to the field of neurology in preclinical years: 42.8% (75/175) “yes”, 28.5% (50/175) “unsure”, and 28.5% (50/175) “no” (Fig. 1C), with 56% (81/151) preferring clinical opportunities, and 22% in mentoring and research (Fig. 1D). We also investigated student’s preferences for different learning methods. This survey found that students felt that among different teaching formats, lectures were the most helpful in aiding understanding of neurology, followed by neurology day (bedside teaching case sessions during the second year NBS course), neuroanatomy lectures, and Problem Based Learning (PBL) case sessions. Data showed that a total of 206,157 M.D. medical students matched into a neurology residency (adult or child) program in the United States during 2011 to 2020, with an annual average of 1.78 ± 0.086% (standard error of the mean). During the same period, 1,363 PSCOM students matched into a neurology residency program with an annual average of 4.05 ± 0.27%. Table 1 shows the match numbers and percentages for each year (z-score 6.34, p < .00001).
Discussion
Early exposure to a specialty of interest is important in training future physicians. Specifically, clinical exposure in preclinical years has been found to significantly influence students’ perceptions and interest in neurology, as these appear to be intertwined with neurophobia6.
Our study showed that PSCOM students perceive a lack of significant exposure to neurology in the critical preclinical years, which could affect student perception about neurology and further amplify the gap. Many students reported an early interest in neurology, but were unaware of how to obtain exposure prior to their preclinical neurosciences course. This lack of awareness likely contributes to first and second year medical students perceiving limited exposure to neurology. In response to these results, the PSCOM Student Interest Group in Neurology (SIGN) chapter incorporated the Early Career Exploration in Neurology Program to provide opportunities for early exposure to neurology, including clinical shadowing experiences. Furthermore, neurology was incorporated into a clinical immersion week, where all first-year students spend a half-day learning about the different neurology subspecialties and clinical neurosciences (localization, neurologic exam, diagnostic testing, etc.). These enhanced programs are consistent with literature demonstrating positive outcomes of students who obtained early exposure, mentorship, and hands-on experiences1.
PSCOM’s neurology match data consistently showed a higher proportion of students matching into neurology from 2011-2020 compared to national data. An exception was in 2017 as the few students that applied to neurology failed to match for unclear reasons. The cause of the neurology match trends at PSCOM are likely multifactorial, with the preclinical curriculum as a major contributor which demystifies neurology and increases student comfort. Prior studies show that increased clinical integration and opportunities to apply neurology, student comfort and interest increases6,8,11.
Landmark changes that likely contributed to the reduction in neurophobia included the implementation of the SIGN in the 1990s and alterations in the preclinical neurosciences course in 2012, which includes clinically oriented neurological cases, the addition of “Neurology Day”, and a neurology examination day during the course. Second year medical students learn basic neuroscience with relevant clinical correlates in an evidence-based learning environment, including problem-based learning (PBL) and flipped classrooms. In third year, knowledge learned in second year is applied to the clinical setting. The integration of these concepts has been shown to help mitigate fears of neurology being complicated and siloed, while reinforcing deeper learning. This is evidenced by a study conducted at the University of Rochester. As described in the article, a 10-week pre-clinical neurology course that involves neurosciences with clinical medicine is integrated throughout. Furthermore, the neurology clerkship boosts learning with other methods such as simulated patient encounters, interdisciplinary conferences, peer teaching and integrated science sessions.
The learning strategies identified in the current study are consistent with those implemented at the University of Rochester, which also has a higher-than-average neurology match rate. The authors of that study attributed their findings to strategies administered to combat neurophobia, which included continued integration of clinical neuroscience material, active learning opportunities, and student engagement6. Additional literature demonstrates factors aside from neurophobia that may influence neurology match rates, including ratings of the neuroscience course or clerkship, the effectiveness of teaching, and a sense of “good fit” with personality, interest, or skills1. Furthermore, students with enthusiastic attitudes toward their neurology clerkship considered the field “more favorably as a possible career”11. These studies again highlight the impact that early exposure with clinical integration has on student interest and engagement with neurosciences. As previously described, the clinical learning opportunities combined with early clinical integration in the second year at Penn State, appear to increase in the third and fourth years, as students reported increased comfort (Survey 2), which ultimately aligns with those found in the studies described here, suggesting that they may contribute to the higher match rate in neurology.
Limitations
Limitations of our study include limited data access to only students who agreed to have their information be publicly available and our small sample size as a single institution and survey response rates. Furthermore, Survey 1 was sent to a small group of students who were mentees of a neurology faculty member. Given the small sample size and structure of survey questions allowing variability, the generalizability of Survey 1 is somewhat limited. Our study also only included data from allopathic (M.D.) matches, not osteopathic (D.O.) matches. Lastly, our study investigated match trends as a surrogate for neurology interest, limiting our ability to account for students that failed to match to neurology.
Conclusion
We sought to understand factors influencing medical students’ interest in neurology after finding a statistically significant higher proportion of neurology matches at PSCOM compared to national data. Contributing factors identified by our survey results that may help mitigate neurophobia include: (1) early introduction of neuroscience in the preclinical years, (2) incorporation of innovative educational programs, such as “Neurology Day” and PBL case sessions, and (3) implementing a Neurology Career Exploration Program. Future studies should include other medical academic centers to assess the generalizability of these results across neurology as a specialty.
Author Information
Corresponding Author
April Henry
april.henry309@gmail.com
Author Contributions
All authors have given approval to the final version of the manuscript.
Funding Sources
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Disclosures
No authors have any disclosures or conflicts of interest at this time.
References
1. Gutmann, L., Cahill, C., Jordan, J. T., Gamaldo, C. E., Santini, V., Ali, I., ... & Smith, A. G. (2019). Characteristics of graduating US allopathic medical students pursuing a career in
neurology. Neurology, 92(17), e2051-e2063.
2. Gilbert, D. L., Horn, P. S., Kang, P. B., Mintz, M., Joshi, S. M., Ruch-Ross, H., & Bale Jr, J. F. (2017). Child neurology recruitment and training: views of residents and child
neurologists from the 2015 AAP/CNS workforce survey. Pediatric neurology, 66, 89-95.
3. Jozefowicz, R. F. (1994). Neurophobia: the fear of neurology among medical students. Archives of Neurology, 51(4), 328-329.
4. Abulaban, A. A., Obeid, T. H., Algahtani, H. A., Kojan, S. M., Al-Khathaami, A. M., Abulaban, A. A., ... & Radi, S. A. (2015). Neurophobia among medical students. Neurosciences Journal,
20(1), 37-40.
5. Schon, F., Hart, P., & Fernandez, C. (2002). Is clinical neurology really so difficult?.
6. Tarolli, C. G., & Józefowicz, R. F. (2018, August). Managing neurophobia: how can we meet the current and future needs of our students?. In Seminars in neurology (Vol. 38, No. 04, pp.
407-412). Thieme Medical Publishers.
7. Pakpoor, J., Handel, A. E., Disanto, G., Davenport, R. J., Giovannoni, G., & Ramagopalan, S. V. (2014). National Survey of UK medical students on the perception of neurology. BMC medical
education, 14(1), 1-5.
8. Albert, D. V., Yin, H., Amidei, C., Dixit, K. S., Brorson, J. R., & Lukas, R. V. (2015). Structure of neuroscience clerkships in medical schools and matching in neuromedicine. Neurology,
85(2), 172-176.
9. Residency Matches - Penn State College of Medicine [Internet]. [cited 2020 Jul 11]. Available from: https://med.psu.edu/md-students/match-list
10. Main Residency Match Data and Reports [Internet]. The Match, National Resident Matching Program. [cited 2020 Jul 11]. Available from: http://www.nrmp.org/main-residency-match-data/
11. Dewey, R. B., & Agostini, M. (2010). Attitudes and performance of third-vs fourth-year neurology clerkship students. Archives of neurology, 67(5), 548-551.
Survey 1: Student Perceptions of Neurology Exposure and Neurological Field
1. Do you feel that you have received adequate teaching in neurosciences?
a. Yes
b. No
2. How would you rate your level of comfort performing the neurological exam?
a. Very comfortable
b. Comfortable
c. Average
d. Uncomfortable
e. Very Uncomfortable
3. Are you considering neurology as specialty?
a. Yes
b. No
4. What opportunities were the most beneficial (free response) in helping your understanding of basic and clinical neuroscience? [free text]
5. Do you feel that your preclinical years adequately integrate clinical neurology?
a. Yes
b. No
6. How satisfied are you with the exposure you have had to neurology as a medical student?
a. More than satisfactory
b. Satisfactory
c. Less than satisfactory
d. None
Survey 2: Neurology Exposure in Preclinical Years
1. What year are you in?
a. MS1
b. MS2
c. MS3
d. MS4
2. How much exposure to neurology did you/are you receiving in your first year & second year prior to the neurology block of medical school?
a. More than satisfactory
b. Satisfactory
c. Less than satisfactory
d. None
3. If you responded with "satisfactory" or "more than satisfactory" to the above question, please identify what type(s) of exposure(s) you had (ex. shadowing, research, SIGN, etc.). One word
answers, phrases, or longer explanations all acceptable.
4. Do you wish there were more opportunities to gain exposure to neurology during your preclinical years (first year & second year prior to neurology block)?
a. Yes
b. No
c. Unsure
5. Do you know where to find opportunities to gain exposure to neurology?
a. Yes
b. No
6. In what areas would you be interested in receiving opportunities in neurology?
a. Clinical: Shadow outpatient clinic/inpatient service
b. Research: Participate in current research in neurology
c. Mentoring: Individual career mentoring via a neurologist