Background
Dyspepsia is a constellation of symptoms ranging from sensations of discomfort, burning, or pain of the upper gastrointestinal tract often in the epigastric region. Symptoms may progress from dyspepsia to peptic ulcer disease (PUD)1. Dyspepsia and PUD can become severe enough to limit daily activities, cause gastrointestinal bleeding, gastric outlet obstruction, perforation, or even death. Common causes of dyspepsia include gastro-esophageal reflux disease and functional dyspepsia. Some of these causes, particularly the acute presentation of PUD, include bleeding, perforation, or obstruction and can be associated with high mortality rates up to 34%2. Globally, the prevalence of dyspepsia is between 11%-29%, with uninvestigated dyspepsia rates suspected to be as high as 45% in some countries2. Low middle-income countries (LMICs) are particularly affected. Known risk factors for dyspepsia include use of non-steroidal anti-inflammatory drugs (NSAIDs), Helicobacter pylori (H. pylori) infection, alcohol use, smoking, and low socioeconomic status3. Although the pool of evidence is limited, previous work has identified that NSAIDs, H. pylori, and socioeconomic status (SES) may play significant roles in dyspepsia in LMICs. Anecdotal studies in urban sub-Saharan Africa (SSA) show that up to 33% of patients presenting with dyspepsia report a history of NSAID use, and dyspepsia in the setting of NSAID use is associated with an increased risk for PUD4. In addition, a cross-sectional study by Archampong et al. conducted in urban Ghana found that H. pylori infection was strongly correlated with dyspepsia and ulcer disease with an odds ratio of 2.4 (p<.05). Additionally, previous studies have shown an inverse association between the prevalence of dyspepsia and markers of SES including educational level3,5.
To date, however, there have been few community-based studies on the prevalence of dyspepsia in African countries, none of which have been performed in Ghana. In the few studies available, dyspepsia prevalence ranges from 26% to 58%6-8. Much of the existing literature focuses on H. pylori infection and endoscopic diagnosis in patients with clinically diagnosed dyspepsia. However, these patients may not be representative of the broader population as they represent the population entering the healthcare system with complicated peptic ulcer disease. Furthermore, these studies characterize patients in urban, tertiary centers, which differ from the rural or suburban community.
The aims of our study are to 1) define the prevalence of dyspepsia, and 2) characterize associated risk factors in a rural SSA setting of Ghana by interviewing randomly selected visitors of patients in the a local regional hospital. To our knowledge, this is the first study to be conducted in this region to characterize dyspepsia and its associated risk factors. We hypothesize that in SSA, a region with limited access to care, the prevalence and risk factors of dyspepsia are unique from higher income countries.
Methods
Subjects
This study was conducted over two weeks at local regional hospital in southern Ghana, in July of 2019. Interviewers worked with local health care providers who served as translators. The questionnaire was administered to 154 visitors of patients. The recruited visitors were not actively seeking care for themselves when recruited. Participants were randomly recruited and interviewed from a variety of departments within the hospital. Only respondents over the age of 18 were eligible to participate.
Questionnaire design
The questions formulated on the questionnaire were driven by the outcomes needed for the study. The scaffolding of the project questionnaire was adapted from the Surgeons OverSeas Assessment of Surgical Needs (SOSAS) in order to standardize collection of demographic data (available at http://www.surgeonsoverseas.org/)9.
The dyspepsia graphics and questions were directly from the Short Form Leeds Dyspepsia Questionnaire (SF-LDQ) by Fraser A et al10. The summed frequency score with a cut-off of 4/16 was used to identify individuals with dyspepsia, which has a sensitivity of 86.0% and a specificity of 66.2%. The SF-LDQ has been proven to be a reliable and accurate tool in measuring the prevalence and severity of dyspepsia in a variety of diverse populations11,12.
Methods of recruitment
Interviewers were paired with native Twi-speaking hospital staff interpreters. This study utilized a convenience sample of randomly selected visitors waiting in different departments at the regional hospital. Participants were approached and the consent form was translated for them and they were asked to participate in the study. Research assistants and bilingual interpreters were present at each interview. Research assistants were trained with the use of the survey, obtaining consent, and managing data. If the respondent consented, they were administered the questionnaire. Inclusion criteria included any visitor (not actively seeking treatment) at the regional hospital over the age of 18 years old. They were excluded if they were being seen as a patient at the hospital, were currently working in the hospital, were younger than 18 years of age, or refused to be part of the study.
Consent and confidentiality
Before the administration of the survey all participants were given an explanation in either English by the research assistant or Twi by the interpreter. If oral consent was given and the participant met the inclusion criteria, written consent was obtained. In cases where the participant was illiterate or unable to sign written documents, their thumbprint was obtained to document consent. All personally identifying information was kept confidential. The interviews took place in a public setting, typically the waiting area of the department in which their family member was seeking care.
Ethical considerations
The study was approved by the ethical review board of the regional hospital and Institutional Review Board at the corresponding author’s institution.
Data analysis/calculations
We reported values as frequencies and percentages for all categorical variables and mean and standard deviation for all continuous variables. The primary outcome of interest was the presence of dyspepsia defined as a score of 4 or higher out of 16 points of the summed frequency score from Short-Form Leeds dyspepsia questionnaire10.
Univariate analysis was performed using the Chi-squared test for categorical variables and Wilcoxon rank-sum test for continuous outcomes to determine factors that were significantly associated with dyspepsia. Variables investigated included age, sex, annual income, insurance status, education level, occupation, cigarette use, alcohol use, NSAID use (defined as current and past use), past ulcer diadiagnosis, previous H. pylori test, history of anemia, history of black or bloody stools, and running water in home.
Variables that were significant in univariate analysis were entered in the multiple logistic regression model while controlling for age and gender to estimate the odds ratio (OR) and 95% confidence interval (95% CI) associated with dyspepsia. Receiver operating characteristic curves were used to quantify the predictive performance of the final model. Statistical analysis was performed using SAS, version 9.4; SAS Institute Inc. and R software (R Core Team 2018). For all statistical tests, alpha level was set at 0.05.
Results
A total of 149 individuals were interviewed for the survey. Summarized in Table 1 are the demographic characteristics of the study participants. The study included 76 female and 73 male participants. The mean age was 40.6 (SD 16.2) years old. Ninety-two (61.7%) reported NSAID use, 32 (21.5%) reported alcohol use, and only 2 of the 149 (1.3%) individuals interviewed reported cigarette use. The overall prevalence of dyspepsia in this sample was 25.5% (38/149) based on the summed frequency from the questionnaire.
Univariate analysis revealed significant association of dyspepsia and cigarette use (p=0.02), education level (p=0.02), NSAID use (p=0.046), previous ulcer diagnosis (p=0.02), and past diagnosis of anemia (p=0.01). No significant association was found for sex (p=0.32), age (p=0.30), annual income (p=0.36), occupation (p=0.49), insurance status (p=0.18), alcohol use (p=0.94), running water in the home (p=0.17), and history of black stools or blood in stools (respectively p=0.42 and p=0.93).
Multivariable logistic regression adjusting for age, gender, NSAID use, education level, and past anemia diagnosis was used to determine the odds ratio of associated dyspepsia (Table 2). Participants with a history of diagnosed anemia were 4.6 times more likely to have dyspepsia (aOR 4.64, 95% CI 1.45 to 15.54, p=0.09). We observed an inverse dose-response relationship between dyspepsia as education level increased. Compared to those who had less than high school education, those who were high school graduates had lower odds of dyspepsia (aOR 0.3, 95% CI 0.10 to 0.89, p=0.03, p for trend < 0.001). Those with greater than a high school education had the lowest odds of dyspepsia (aOR: 0.22, 95% CI 0.06 to 0.46, p=0.03). NSAID use was associated with an odds-ratio of 2.16 (OR 2.16; 95% CI 0.91 to 5.55, p=0.09), however, this result did not reach statistical significance. Age and gender were not statistically associated with dyspepsia on multivariable analysis.
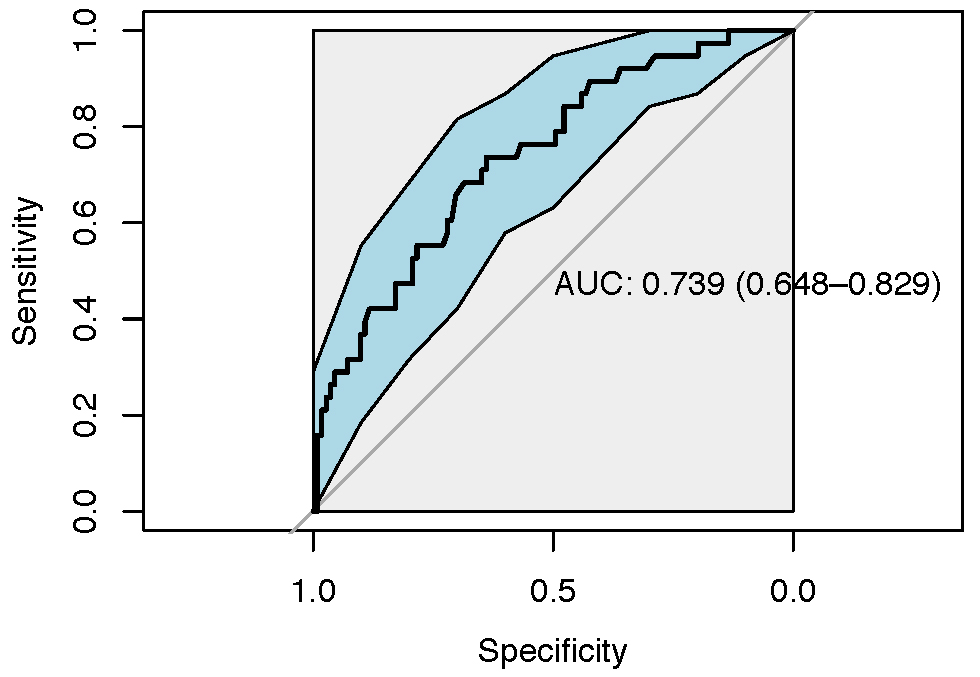
The model that included the history of anemia, age, education, and NSAID use predicted 74% of participants with dyspepsia, with AUC of 0.74, Figure 1.
Figure 1. Predictive performance of the predictive modeling for predictors of dyspepsia. This model could predict 74% of the dyspepsia patients using the previous history of anemia, education, age, and NSAID use.
Discussion
This community-based study found a prevalence of dyspepsia of 25.5% in the Eastern Region of Ghana. Our study found significant associations of individual risk factors in addition to pertinent medical history findings to aid in diagnosis of dyspepsia. Individual modifiable risk factors associated with dyspepsia included cigarette use and NSAID use. While tobacco use was reported to be a rare exposure in this population, on univariate analysis it was strongly correlated to a diagnosis of dyspepsia. The low prevalence of tobacco use in Ghana has been previously documented to be lower than many other LMICs, likely from long-standing limitations that have been placed on tobacco advertisement13. Additionally, there are well recognized public health campaigns supporting smoke-free policies and public education on the health effects of smoking including cardiovascular, lung, oral and throat cancer14. Unfortunately, the risks of dyspepsia and PUD are not currently included as a health consequence of tobacco use in educational public health campaigns. Given the tangibility and immediate discomfort associated with dyspepsia as compared to cardiovascular disease or cancer, which are long-term and more theoretical for current smokers, education surrounding the association of tobacco use with dyspepsia could serve as a useful tool to further decrease tobacco use in Ghana.
NSAID use was more common than tobacco use, with 21.5% of respondents using NSAIDs in our study. Despite high documented prevalence of NSAID use between 32.6%4 to 66%15 in those with documented PUD, because of the availability of NSAIDs and NSAID containing over the counter products, the prevalence of use in rural Ghana is not well documented. Previous studies have found that users of over the counter analgesia are frequently unaware of both recommended dose and potential side-effects leading to frequent overuse and misuse16. Education, both on an individual healthcare provider level and as public outreach, surrounding proper use and associated risks of NSAIDs is an important public health issue that could impact dyspepsia and PUD morbidity in Ghana.
The inverse relationship between education level and dyspepsia is an interesting, but not a surprising finding in this study. The protective association (OR 0.3 and 0.22), as well as the dose-response relationship (the more education, the less likely to suffer from dyspepsia), imply a strong relationship between education and dyspepsia identified in this study. While education level had a strong relationship, interestingly, annual income was not associated with dyspepsia symptoms. The lack of statistical significance of the relationship between income and dyspepsia could be due to a large number (29) of individuals unable to report their annual income resulting in unknown incomes. This relationship between dyspepsia and education and income calls into question the overall role of socioeconomic status in dyspepsia. Studies performed elsewhere have had similar mixed results with many studies finding no association between socioeconomic status and dyspepsia2. However, studies performed in Canada and Britain found a similar relationship with low education levels predictive of dyspepsia3,5. While not measuring education or income directly, a study performed in Nigeria found an association between occupational scatter and large family size associated with dyspepsia, which is suggestive of socio-economic determinants of dyspepsia in this region17. Overall, results of previous studies in conjunction with the results from this study suggest that there is likely an association of socio-economic factors and prevalence of dyspepsia in both high and low-middle income countries. Future research is needed to further understand the complex relationship of socio-economic factors, such as education level and household income, and dyspepsia prevalence and symptoms in different environments.
Additional important findings in this study were the strong association of a diagnosis of anemia and previous ulcer diagnosis with current dyspepsia symptoms. This finding suggests that patients with symptoms of dyspepsia and PUD are likely not receiving adequate treatment to resolve their symptoms or are at high risk for recurrence. However, this study is cross-sectional in nature, and the temporal relationship cannot be determined. Despite this, health care providers should be aware of the association of patients with past ulcers and diagnosis of anemia and the association of dyspepsia. This information can be used by general practitioners and primary care doctors to appropriately screen high-risk patients for dyspepsia and potentially identify dyspepsia and PUD before progression occurs.
While a definitive diagnosis of dyspepsia and PUD often rely on laboratory tests as well as endoscopic evaluation of the upper GI tract, few patients and facilities have the resources to undergo definitive testing. Many previous studies of incidence of dyspepsia and PUD rely on invasive endoscopic testing as well as laboratory testing for H. pylori to confirm diagnosis15. Tabiri et al. found that cigarette use, alcohol use, and NSAIDs were associated with gastric ulcer on EGD. From our population-based survey, we also found NSAID and cigarette use to be independently associated with self-reported dyspepsia symptoms. Our study did differ in that alcohol use was not significantly associated with dyspepsia. However, Tabiri et al. had a higher cut off of five alcoholic drinks per day. Overall, this reinforces the importance of medical history in making accurate medical diagnosis of both dyspepsia and PUD. The similarities of our demographic findings further validate the accuracy of questionnaires and history to make a diagnosis of dyspepsia when specialized tests such as endoscopy and H. pylori lab testing are unavailable or would significantly delay treatment, especially in a low resource environment such as rural Ghana.
Late presentation of disease is a significant problem in rural LMICs. Studies found that patients in other rural areas of Ghana delay over 22 months from symptom onset until presentation to a medical facility.18 Many diseases that could easily be treated medically in early-stage progress to cause significant surgical disease resulting in morbidity and mortality. Dyspepsia and peptic ulcer disease are a prime example in rural Ghana. While dyspepsia typically responds to medical treatment, if left untreated it can progress to peptic ulcer disease that can result in perforation with mortality rates of up to 35%19. Our study looks to identify patients very early in their presentation, with summed frequency scores as low as 4 (range 4-14). This study shows that early identification of dyspepsia on a community level is possible. Early detection and treatment have the potential to decrease late presentation that is associated with morbidity and mortality.
A strength of this study is the approach from a community level, which has not been previously performed in this population. We interviewed and obtained data from individuals who were not actively seeking treatment. This gives the perspective of the baseline burden within the community as opposed to sampling from a population actively seeking care. This study is especially valuable to Eastern Regional Hospital to both help screen patients and identify those with dyspepsia and potentially prevent more severe PUD morbidity and mortality. The use of specific screening characteristics known to be associated with dyspepsia gives insight into the potential for a preventive approach to dyspepsia and peptic ulcer disease as opposed to a hospital-based, reactionary approach once the disease progresses and becomes a medical emergency in the form of perforation, gastrointestinal bleed, or obstruction.
Limitations
This study is not without limitations. One limitation of this study is that the data was self-reported was not verified by medical records. Some individuals were unclear of past diagnosis or treatments of dyspepsia, ulcers, and H. pylori which represents some inherent recall bias. Additionally, while we did use a verified dyspepsia questionnaire, confirmatory testing with endoscopy or H. pylori lab testing was unable to be completed. Future work surrounding the burden of dyspepsia in this region will include investigation of H. pylori burden as well as risk factors for advanced disease with a focus on PUD and its surgical complications which is the outcome with the highest morbidity and mortality. In addition, it is important to note when considering results of this study that interviews did take place in public setting. While every opportunity to conduct interviews privately was taken, it is possible that subjects may have adjusted answers with a potential for unpredictable skew of results. Although it was clearly expressed to all participants that they could withdraw from the study at any time.
Conclusion
Dyspepsia, as diagnosed from self-reported questionnaires, has a high prevalence in Eastern Ghana with risk factors and associations like other parts of the country and other LMICs. These risk factors include tobacco use, NSAID use, low education level, and previous diagnosis of anemia and prior ulcers. Recognition of dyspepsia can be made at the community level with minimal resources and could potentially serve as a way to identify disease and direct intervention for dyspepsia and PUD.
Author Information
Corresponding Author
*Elizabeth Olecki, MD
eolecki@pennstatehealth.psu.edu
Author Contributions
All authors have given approval to the final version of the manuscript.
Funding Sources
The authors received no financial support for the research, authorship, and/or publication of this article.
Disclosures
No authors have any disclosures or conflicts of interest at this time.
Acknowledgements
We would like to acknowledge Dr. Cardinal Newton, Clinical Director for Easter Regional Hospital.
References
1. Talley NJ, Ford AC. Functional Dyspepsia. N Engl J Med. 2015;373(19):1853-63.
2. Mahadeva S, Goh KL. Epidemiology of functional dyspepsia: a global perspective. World J Gastroenterol. 2006;12(17):2661-6.
3. Moayyedi P, Forman D, Braunholtz D, Feltbower R, Crocombe W, Liptrott M, et al. The proportion of upper gastrointestinal symptoms in the community associated with Helicobacter pylori, lifestyle factors, and nonsteroidal anti-inflammatory drugs. Leeds HELP Study Group. Am J Gastroenterol. 2000;95(6):1448-55.
4. Archampong TN, Asmah RH, Wiredu EK, Gyasi RK, Nkrumah KN. Factors associated with gastro-duodenal disease in patients undergoing upper GI endoscopy at the Korle-Bu Teaching Hospital, Accra, Ghana. Afr Health Sci. 2016;16(2):611-9.
5. Tougas G, Chen Y, Hwang P, Liu MM, Eggleston A. Prevalence and impact of upper gastrointestinal symptoms in the Canadian population: findings from the DIGEST study. Domestic/International Gastroenterology Surveillance Study. Am J Gastroenterol. 1999;94(10):2845-54.
6. Bitwayiki R, Orikiiriza JT, Kateera F, Bihizimana P, Karenzi B, Kyamanywa P, et al. Dyspepsia prevalence and impact on quality of life among Rwandan healthcare workers: A cross-sectional survey. S Afr Med J. 2015;105(12):1064-9.
7. Holcombe C, Omotara BA, Padonu MK, Bassi AP. The prevalence of symptoms of dyspepsia in north eastern Nigeria. A random community based survey. Trop Geogr Med. 1991;43(1-2):209-14.
8. Lee YJ, Adusumilli G, Kyakulaga F, Muwereza P, Kazungu R, Blackwell TS, et al. Survey on the prevalence of dyspepsia and practices of dyspepsia management in rural Eastern Uganda. Heliyon. 2019;5(6):e01644.
9. Fuller AT, Butler EK, Tran TM, Makumbi F, Luboga S, Muhumza C, et al. Surgeons OverSeas Assessment of Surgical Need (SOSAS) Uganda: Update for Household Survey. World J Surg. 2015;39(12):2900-7.
10. Fraser A, Delaney BC, Ford AC, Qume M, Moayyedi P. The Short-Form Leeds Dyspepsia Questionnaire validation study. Aliment Pharmacol Ther. 2007;25(4):477-86.
11. Gatta L, Moayyedi P, Tosetti C, Vakil N, Ubaldi E, Barsanti P, et al. A validation study of the Italian Short-Form Leeds Dyspepsia Questionnaire. Intern Emerg Med. 2010;5(6):501-6.
12. Mahadeva S, Chan WK, Mohazmi M, Sujarita R, Goh KL. Validation study of the Leeds Dyspepsia Questionnaire in a multi-ethnic Asian population. J Gastroenterol Hepatol. 2011;26(11):1669-76.
13. Yawson AE, Baddoo A, Hagan-Seneadza NA, Calys-Tagoe B, Hewlett S, Dako-Gyeke P, et al. Tobacco use in older adults in Ghana: sociodemographic characteristics, health risks and subjective wellbeing. BMC Public Health. 2013;13:979.
14. Owusu-Dabo E, Lewis S, McNeill A, Gilmore A, Britton J. Support for smoke-free policy, and awareness of tobacco health effects and use of smoking cessation therapy in a developing country. BMC Public Health. 2011;11:572.
15. Tabiri S, Akanbong P, Abubakari BB. Assessment of the environmental risk factors for a gastric ulcer in northern Ghana. Pan Afr Med J. 2016;25:160.
16. Badzi CD, Ackumey MM. Factors influencing use of analgesics among construction workers in the Ga-Eastmunicipality of the Greater Accra region, Ghana. Ghana Med J. 2017;51(4):156-63.
17. Ihezue CH, Oluwole FS, Onuminya JE, Okoronkwo MO. Dyspepsias among the highlanders of Nigeria: an epidemiological survey. Afr J Med Med Sci. 1996;25(1):23-9.
18. Tabiri S, Jalali A, Nelson RE, Damah MC, Abantanga FA, Price RR, et al. Barriers to Timely Presentation of Patients with Surgical Conditions at Tamale Teaching Hospital in Northern Ghana. World J Surg. 2019;43(2):346-52.
19. Rickard J. Surgery for Peptic Ulcer Disease in sub-Saharan Africa: Systematic Review of Published Data. J Gastrointest Surg. 2016;20(4):840-50.
