Image Challenge (archive)
Image Challenge: Special Holiday Edition - Friday, December 25, 2020

A previously healthy 25-year-old woman presented with a 4-day history of a swollen and red right upper eyelid with 3 out of 10 pain. The eyelid swelling has progressively worsened, and she has had tearing from the right eye. She reported no recollection of getting bitten or other trauma and denies fever, chills, pain with eye movement, vision loss, double vision or other change in vision, or itchiness. She has worn soft disposable contact lenses since the age of 16, and she reports no history of sinusitis or recent nasal discharge as well as no significant family history of eye disease. What is the most likely diagnosis?
A) Blepharitis
B) Insect Bite
C) Orbital Cellulitis
D) Preseptal Cellulitis
E) Viral Conjunctivitis
Correct Answer: D) Preseptal Cellulitis
Incorrect Answers:
A) Blepharitis is an ophthalmologic condition identified by inflammation of the eyelid margin. Presentation involves bilateral red, swollen, or itchy eyelids with crusting or flakes of the eyelid skin. The standard treatment includes warm compresses and artificial tears for mild cases. For more severe cases, topical antibiotic and/or anti-inflammatory agents is recommended. [1]
B) An insect bite usually causes local allergic reactions from the punctured area due to an immunological response to proteins in mosquito saliva. Symptoms consist of an itchy and/or painful area of redness, warmth, and swelling. Treatment of allergic reactions from insect bites may include antihistamines. [2]
C) Orbital cellulitis is an infection involving the muscles and fat that is found within the orbit of the eye. Presentation includes eyelid swelling and erythema with ocular pain, blurred and/or double vision, fever, pain with eye movement, and restricted eye movement. Treatment for orbital cellulitis includes broad-spectrum intravenous antibiotics to cover Gram-positive, Gram-negative, and anaerobic organisms for 48 to 72 hours, followed by oral antibiotics for at least a week. Surgery may be needed in select cases, such as if the orbit is tight, an optic neuropathy is present, or the intraocular pressure is severely elevated. [3]
E) Viral conjunctivitis, sometimes referred to as “pink eye,” is a common inflammation of the mucous membrane inside the surface of the eyelid from an adenovirus. Presentation includes morning crusting, daytime redness, and watery discharge. Management of viral conjunctivitis includes measures to prevent the spread of this highly contagious condition (e.g., frequent handwashing and avoid touching eyes, shaking hands, sharing towels or pillows), artificial tears and cool compresses. Topical antihistamine drops may be helpful if itching is severe, and topical steroids may be indicated in select cases (e.g., if a membrane/pseudo-membrane is present). [4]
Preseptal Cellulitis
Loriel Arcangel, BS and Ingrid U. Scott, MD, MPH
A previously healthy 25-year-old woman presented with a 4-day history of a swollen and red right upper eyelid with 3 out of 10 pain. The eyelid swelling has progressively worsened, and she has had tearing from the right eye. She reported no recollection of getting bitten or other trauma and denies fever, chills, pain with eye movement, vision loss, double vision or other change in vision, or itchiness. She has worn soft disposable contact lenses since the age of 16, and she reports no history of sinusitis or recent nasal discharge as well as no significant family history of eye disease. On her eye examination, a swollen, erythematous, tender right upper eyelid with watery discharge was observed. There was no proptosis (protrusion or displacement of the eye), no restriction of eye movement, and no abnormality of the pupils in response to light. A diagnosis of preseptal cellulitis was made clinically. Augmentin (amoxicillin-clavulanic acid) was recommended, and the patient’s symptoms improved over the next few days.
Preseptal cellulitis, also known as periorbital cellulitis, is most commonly caused by Staphylococcus aureus or Streptococcus. However, Haemophilus influenzae should be considered in non-immunized children, and anaerobes should be suspected if there is foul-smelling discharge, necrosis, or a history of an animal or human bite. Preseptal cellulitis is characterized by unilateral ocular pain, eyelid swelling, erythema, and tenderness. Orbital cellulitis should be suspected if there is ophthalmoplegia, proptosis, an afferent pupillary defect, dyschromatopsia, or pain with eye movement. Several epidemiologic studies have reported that preseptal cellulitis is more common in children than adults. Adults and children who are older than 5 years of age can usually be managed on an outpatient basis with antibiotics for five to seven days if the patient has no signs of systemic toxicity. A computed tomography (CT) scan of the brain and orbits (axial and coronal views) with contrast should be performed if there is a history of significant trauma or a concern about a possible orbital or intraocular foreign body, orbital cellulitis, subperiosteal abscess, paranasal sinusitis, cavernous sinus thrombosis, or malignancy. [5] A complete blood count with differential and blood cultures should be considered in severe cases or when fever is present. Children who are under 5 years of age, patients who are severely ill or noncompliant with outpatient treatment and follow-up, and patients with no noticeable improvement or with a worsening condition after 24 to 48 hours of oral antibiotics should be admitted to the hospital and treated with broad-spectrum intravenous antibiotics and undergo a CT scan to assess for orbital cellulitis. [3]
References:
1. Shtein RM. Blepharitis. UpToDate. 2020.
2. Kelso JM. Allergic reactions to insect bites. UpToDate. 2020.
3. Gappy C, Archer SM, Barza M. Preseptal and orbital cellulitis. UpToDate. 2020.
4. Jacobs DS. Conjunctivitis. UpToDate. 2020.
5. Gerstenblith AT and Rabinowitz MP, editors; Barahimi BI and Fecarotta CM, associate editors. The Wills Eye Manual. Office and Emergency Room Diagnosis and Treatment of Eye Disease, sixth edition. Wolters Kluwer, Lippincott Williams & Wilkins, Philadelphia, 2012.
Image Challenge: Week 37 - Friday, December 18, 2020

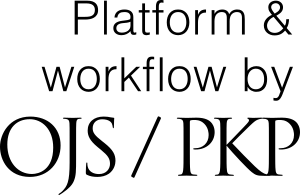
A 23-year-old healthy Asian female presents to the clinic for an evaluation of a light brown, dry, painless, raised spot on her right upper back that she noticed 4 months ago. Patient reports she noticed it after a day at the beach and is concerned about skin cancer. She also states she has been going to the gym more frequently and thought it may be a result of staying in sweaty clothes for a long time. She denies fever, pain, redness, swelling, and itching. The patient states the lesion has not grown in size and she has not applied or taken any topical or oral medications, respectively. The patient is adopted, and the family history is unknown. On the physical exam, there are multiple 0.2 mm waxy light brown colored slightly raised lesions in a group with a “stuck-on” appearance. There is no pain, erythema, warmth, or pus at the site. What is the most likely diagnosis?
A) Basal cell carcinoma
B) Nevi
C) Milia
D) Seborrheic keratosis
E) Verruca vulgaris
Correct Answer: D) Seborrheic Keratosis
Incorrect Answers:
A) Basal cell carcinoma (BCC) is a malignant neoplasm of the basal cells of the epidermis. BCC is the most common human malignant disease usually found on sun-exposed skin because ultraviolet radiation is responsible for most cases particularly in patients who have fair skin, blue eyes, and/or red hair. A “pearly” appearance is a characteristic feature of most cases. Four distinct types of BCC include nodular, pigmented, superficial and sclerotic. Although these lesions rarely metastasize, patients should seek medical attention if there is family history of skin cancer or if any changes are noticed in the growth.
B) A nevus is a mole of pigment forming cells, the nevus cell. Nevi is a normal skin finding people develop as early as 6 months of age and continue to develop until they are around 65 years old. Most people have approximately 15-40 nevi that are brown with a uniform color, surface and border. Nevi can appear all over the body, but any unusual lesion with a different color or texture should be biopsied to rule out potential malignancies.
C) Milia are small, superficial epidermal keratin cysts often found on the face that arise from pilosebaceous units or eccrine sweat ducts. Milia are 1-2mm in diameter and present as firm white papules. Most often they develop spontaneously at all ages but can develop when burns are healing. There is no treatment necessary for milia, but topical retinoids or incisions can be used for cosmetic reasons.
E) Verruca Vulgaris (VV), also known as the common wart is a small painless flesh-colored firm papule. The skin lines are interrupted and studded with black puncta which look like small dots at the base of the papule. VV is caused by various strains of human papillomavirus. While different strains cause warts in different parts of the body, the hands and digits are the usual sites. While treatment is not necessary, topical Salicylic acid and cryotherapy with liquid nitrogen are commonly used.
Seborrheic Keratosis
Bao Sciscent, BS; Matthew F. Helm, MD; Alexandra Flamm, MD; Joslyn Sciacca Kirby, MD; Brian Green, DO
A 23-year-old healthy Asian female presents to the clinic for an evaluation of a light brown, dry, painless, raised spot on her right upper back that she noticed 4 months ago. Patient reports she noticed it after a day at the beach and is concerned about skin cancer. She also states she has been going to the gym more frequently and thought it may be a result of staying in sweaty clothes for a long time. She denies fever, pain, redness, swelling, and itching. The patient states the lesion has not grown in size and she has not applied or taken any topical or oral medications. The patient is adopted, and the family history is unknown. On the physical exam, there are multiple 0.2 mm waxy light brown colored slightly raised lesions in a group with a “stuck-on” appearance. There is no pain, erythema, warmth, or pus at the site. Based on the clinical appearance and past medical history, the diagnosis of seborrheic keratosis was made, and treatment was not recommended. Since the initial visit, there have been no changes in size, texture, or color, and there is still an absence of any irritation.
Seborrheic keratosis is a common skin growth due to benign proliferation of immature keratinocytes that is often seen in older people. They vary in size from 2mm to 2cm and are often skin colored, light brown, or tan and commonly appear on the trunk, face, and upper extremities. [1] Familial inheritance and pathogenesis of this condition are not known at this time although there is belief of a genetic component and activating mutations for its development. [2] The diagnosis is made on clinical appearance. Most of the time, they do not cause any symptoms and therefore do not require treatment unless there is constant irritation due to friction that can occur based on the location of the lesion or for cosmetic reasons. If the growth is bothersome, treatments include cryotherapy, curettage, and electrodessication. [3]
References:
1. Marks J G, Miller J J. Lookingbill and Marks Principles of Dermatology, 6e. Philadelphia: Elsevier. 2019.
2. Greco M, Bhutta B. Seborrheic Keratosis. StatPearls. 2020.
3. Goldstein B, Goldstein A. Overview of benign lesions of the skin. UpToDate. 2020.
Image Challenge: Week 36 - Friday, December 11, 2020

A 57-year-old male with no previous past medical history was referred to dermatology for evaluation of a lesion in the right inguinal area. The patient reports first noticing a small mass 1.5 years ago. It remained stable and asymptomatic for one year. The mass then increased in size over 3 months. During that time, the patient lost 30 pounds and had progressively worsening pain from the mass that made it difficult to walk up the stairs. He was placed on prednisone and oxycodone for what was deemed an inflammatory pseudotumor. Since then, he continues to have worsening pain, but no other symptoms. On physical exam there is a 9 cm wide bright red indurated plaque extending from the right inguinal to suprapubic area with small amounts of tan crust and yellow exudate. There is also an ill-defined pink patch on the inferior border of the inguinal fold that is not continuous with the primary lesion. A biopsy was performed, revealing horseshoe shaped nucleoli in the atypical cells. Immunohistochemical staining was largely positive for CD30 and ALK-1. What is the most likely diagnosis?
A) Anaplastic Large Cell Lymphoma
B) Herpes Zoster
C) Kaposi Sarcoma
D) Mycosis Fungoides
E) Tinea Cruris
Correct Answer: A) Anaplastic Large Cell Lymphoma
Incorrect Answers:
B) Herpes Zoster, colloquially known as shingles, is the reactivation of the varicella zoster virus (VZV). Patients are typically exposed to the virus early in life. The virus will lay dormant in the dorsal sensory root ganglia near the spinal cord. The chances of reactivation increase with age and presents with pain for some days followed by erythematous papules and vesicles in a dermatomal pattern. The most common dermatomes for reactivation are thoracic (55%) followed by cervical (20%). The cutaneous findings usually last for several days before resolving in immunocompetent patients. Post herpetic pain can linger afterwards. Persistent pain beyond one month is seen in less than 2% of patients under age 40, but in up to 75% age 70 and above. Independent of age, the pain gets better with time and is uncommon to last longer than one year. [1]
C) Kaposi sarcoma (KS) is a vascular malignancy. Multiple subtypes exist, such as classic, AIDS-associated, and immunosuppression-associated. Human Herpes Virus 8 can be isolated from KS irrespective of type. The most common type of KS in the United States is AIDS-associated KS secondary to poorly controlled HIV infection. This KS subtype typically favors the head, neck, trunk, and mucous membranes and presents as purple/red macules that progress to papules, nodules, and plaques. The progression of AIDS-associated KS is rapid, but rarely fatal, unlike other types of KS. [1]
D) Mycosis fungoides (MF) is the most common type of cutaneous T cell lymphoma. It is twice as common in men than women. MF has a predilection for the trunk but can be found anywhere on the skin. The clinical presentation of MF usually begins as a single, pruritic patch that is non-specific and can easily mimic more common diagnoses, such as eczema. With time, in some cases the patches can progress to infiltrative plaques and tumor formation. When tumors develop or spread to lymph nodes occur, MF can be fatal. In the early stages of disease, diagnosis can be made from skin biopsy, but is difficult and requires experienced dermatopathologists that can identify its cardinal features. In the advanced stages of disease, diagnosis can be made from lymph node biopsies, flow cytometry, and gene rearrangement testing of biopsies. [1]
E) Tinea is a cutaneous fungal infection caused by dermatophytes. Tinea has different names depending on the location of the body that is involved. Tinea cruris, also referred to as jock itch, is a dermatophyte infection of the groin. Involved areas appear as erythematous, annular scaling patches that spread peripherally. Tinea infections tend to be asymptomatic, but some can itch. Potassium hydroxide drops applied to scale from tinea lesions should reveal hyphae under the microscope and confirm diagnosis. [1]
Anaplastic Large Cell Lymphoma
Ramon Govea, BS; Matthew F. Helm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD; Alexandra Flamm, MD
A 57-year-old male with no previous past medical history was referred to dermatology for evaluation of a lesion in the right inguinal area. The patient reports first noticing a small mass 1.5 years ago. It remained stable and asymptomatic for one year. The mass then increased in size over 3 months. During that time, the patient lost 30 pounds and had progressively worsening pain from the mass that made it difficult to walk up the stairs. He went to the hospital where skin biopsies revealed large, pleomorphic, multinucleated epithelioid appearing cells. He was placed on prednisone and oxycodone for what was deemed an inflammatory pseudotumor. Since then, he continues to have worsening pain, but no other symptoms. On physical exam there is a 9 cm wide bright red indurated plaque extending from the right inguinal to suprapubic area with small amounts of tan crust and yellow exudate. There is also an ill-defined pink patch on the inferior border sparing the skin fold. A biopsy of the skin was inconclusive and surgical biopsy was scheduled one week later, revealing horseshoe shaped nucleoli in the atypical cells. Immunohistochemical staining was largely positive for CD30 and ALK-1. The diagnosis of anaplastic large cell lymphoma was made. The patient was promptly referred to hematology/oncology where staging was performed and the patient initiated treatment with Brentuximab, a monoclonal antibody targeting CD30.
Primary cutaneous anaplastic large cell lymphoma (ALCL) is classified as a type of primary CD30+ cutaneous T cell lymphoma/lymphoproliferative disorder (pcCTCL). These are the second most common CTCLs after mycosis fungoides (MF). The classic presentation of is of a solitary red tumor up that grows up to 10 cm in diameter. These lesions can occur anywhere on the body and tends to ulcerate, regress, and relapse. Since the vast majority of CTCLs are MF, it is important to rule this out before proceeding to the diagnosis of ALCL. Once MF is excluded, the next important evaluation is that of CD30 expression. ALCL is characterized by >75% of anaplastic tumor cells expressing CD30. Prognosis of ALCL depends on multiple factors, one of which is ALK-1. ALCL with negative ALK-1 has a favorable prognosis with irradiation of lesions and low dose methotrexate to prevent relapses. Systemic CD30+ CTCL with cutaneous involvement like the case presented here has a poorer prognosis that becomes slightly better when positive for ALK-1. [1]
Lymphomatoid papulosis (LyP) is another type of CD30+ lymphoproliferative disorder that can mimic ALCL in a few ways. ALCL can present before, at the same time, or after LyP and be almost identical histologically. The clinical presentation of LyP can be similar as well but has a few key differentiating characteristics. When it comes the course of the disease, LyP lesions occur over days to weeks and spontaneously heal, which is not the case in ALCL. A second key difference is the number of lesions. LyP on average has 10-20 lesions at any given time and rarely ever has solitary lesions. One final distinguishing factor is that the lesions in LyP are about 1 cm in diameter and become necrotic before healing as opposed to ALCL lesions that progressively expand in size well past 1 cm and do not typically necrose or heal without treatment. [1]
Reference:
1. James, W. D., Berger, T. G., & Elston, D. M. (2016). Andrews' diseases of the skin: Clinical dermatology. Philadelphia, PA: Elsevier.
Image Challenge: Week 35 - Friday, December 4, 2020

A 26-year-old Asian male with no significant past medical history developed a rash on his chest that has spread to his neck and upper abdomen. The rash is pruritic but not painful. The pruritus is worsened by exercise and sweat. He tried over the counter hydrocortisone cream without relief. He had undergone a strict dietary change one month ago, and maintains a diet consisting of high fats, moderate proteins, and less than ten grams of carbohydrates daily. He has no known allergies and takes no medications. He denies any recent travel or outdoor hiking. On exam, there are pink-tan macules coalescing into patches on his neck, chest, and back. What is the most likely diagnosis?
A) Allergic Contact dermatitis
B) Confluent and reticulated papillomatosis
C) Leukocytoclastic vasculitis
D) Prurigo pigmentosa
E) Subacute cutaneous lupus erythematosus
Correct Answer: D) Prurigo pigmentosa
Incorrect Answers:
A) Allergic contact dermatitis (CD) is characterized by erythema, pruritus, and vesiculation due to direct contact with environmental substances, including poison ivy, soap, or jewelry. Prior sensitization to allergen is needed. Upon re-exposure to low concentrations of the allergen, a type IV hypersensitivity cellular immune response occurs. Acute CD present as small fluid filled vesicles that appear within a few hours of exposure. Chronic CD can manifest as fissuring, skin thickening, and acneiform eruptions. [1]
B) Confluent and reticulated papillomatosis (CARP) is characterized by multiple 1-5mm hyperkeratotic, scaly macules or papules that coalesce to form patches or plaques centrally, and a reticular pattern peripherally. These lesions usually originate in the chest, neck, and axillae and are rarely pruritic. This condition often arises in pubertal age young adults and is most common in Caucasians. While the cause of CARP remains unclear, it is believed to be caused by a skin infection. Dietzia papillomatosis, a gram-positive aerobic actinomycete, is the leading infectious candidate. [2]
C) Leukocytoclastic vasculitis (LCV) is inflammation of small blood vessels that manifests as purple-red palpable purpuric papules. This is commonly found as grouped lesions on the lower legs and other dependent areas, and less frequently found on the upper body. These skin lesions are usually asymptomatic but can be itchy or painful. This condition affects both sexes equality and all ages. [3]
E) Subacute cutaneous lupus erythematosus (SCLE) lesions are characterized as papulosquamous or annular plaques with raised erythematous borders. The lesions are often symmetrically distributed on sun-exposed areas of the neck, upper trunk, and outer arms, and the face is usually unaffected. This condition is most often diagnosed in Caucasian women of 30 to 40 years of age. Up to 30% of SCLE are drug-induced, such as by thiazide diuretics, calcium channel blockers, terbinafine, and chemotherapy agents. [4]
Prurigo pigmentosa
Lisa Ho, BS; Matthew F. Helm, MD; Alexandra Flamm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD
A 26-year-old Asian male with no significant past medical history developed a rash on his chest that has spread to his neck and upper abdomen. The rash is pruritic but not painful. The pruritus is worsened by exercise and sweat. He tried over the counter hydrocortisone cream without relief. He had undergone a strict dietary change one month ago, and maintains a diet consisting of high fats, moderate proteins, and less than ten grams of carbohydrates daily. He has no known allergies and takes no medications. He denies any recent travel or outdoor hiking. On exam, there are pink-tan macules coalescing into patches on his neck, chest, and back. The diagnosis of prurigo pigmentosa is made clinically with patient history and physician exam. The patient had been following an aggressive ketogenic diet. Upon termination of the ketogenic diet and resumption of a higher carbohydrate diet, the skin lesion spontaneously resolved after.
Prurigo pigmentosa (PP) is a rare inflammatory skin disorder with an unknown cause. Systemic conditions such as H. pylori infection, Sjogren’s syndrome, adult-onset Still’s disease, and conditions causing ketosis have been associated with PP. The ketogenic diet has been frequently linked to PP development, as it induces hepatic production of ketone bodies as an alternative fuel source to cause a state of ketosis. PP can be characterized into three stages based on appearance and pathology. Early-stage lesions present as pruritic urticarial plaques or papules with perivascular neutrophilic infiltrates. Fully developed PP lesions present as crusted erythematous papules with necrotic keratinocytes. Late-stage lesions evolve into smooth-surfaced pigmented macules with spongiosis of the epidermis and lymphocytic infiltrate. [5] PP can be successfully treated with dapsone and tetracycline antibiotics during the inflammatory phase of the disease by interfering with the function of neutrophils, and the addition of carbohydrates to the diet for patients who follow a ketogenic diet. [6]
References:
1. Moore A. Contact Dermatitis. The American Academy of Allergy, Asthma & Immunology. Published 2020. https://www.aaaai.org/conditions-and-treatments/library/allergy-library/contact-dermatitis.
2. Ngan V, Stewart T, Oakley A. Confluent and reticulated papillomatosis. DermNet NZ. Published 2018. Dermnetnz.org. https://dermnetnz.org/topics/confluent-and-reticulated-papillomatosis/.
3. Einhorn J, Levis JT. Dermatologic Diagnosis: Leukocytoclastic Vasculitis. Perm J. 2015;19(3):77-78. doi:10.7812/TPP/15-001
4. Gordon H, Oakley A. Subacute cutaneous lupus erythematosus. DermNet NZ. Published July 2019. Dermnetnz.org. https://dermnetnz.org/topics/subacute-cutaneous-lupus-erythematosus/.
5. Alshaya MA, Turkmani MG, Alissa AM. Prurigo pigmentosa following ketogenic diet and bariatric surgery: A growing association. JAAD Case Rep. 2019;5(6):504-507. Published June 2019. doi:10.1016/j.jdcr.2019.03.011
6. Maco MW, Lee E, Wu Y, Lee R. Treatment of Prurigo Pigmentosa with Diet Modification: A Medical Case Study. Hawaii J Med Public Health. 2018;77(5):114-117.
Image Challenge: Week 34 - Friday, November 27, 2020

A 50-year-old female presents with intermittent pain and swelling of the bilateral lower legs which have been occurring for the last 5-6 years. The patient describes the pain as a feeling of pressure and slight burning in her legs, mostly occurring after long periods of standing, walking, or during menstruation. Her pain is relieved by sitting, elevating legs, or wearing compression stockings. Her past medical history includes open-heart surgery for mitral valve prolapse. She says her older sister has similar symptoms in her legs. What is the most likely diagnosis?
A) Cellulitis
B) Deep Vein Thrombosis
C) Hereditary Hemorrhagic Telangiectasia
D) Stasis Dermatitis
E) Varicose Veins
Correct Answer: E) Varicose Veins
Incorrect Answers:
A) Cellulitis is a deep infection of the skin resulting in a localized area of erythema. Common infectious organisms include S. aureus and S. pyogenes. Presentation often involves fever and inflammation of the skin. A history of trauma or a preceding infected skin lesion is sometimes present. In adults, cellulitis most often affects the lower legs. Skin and blood cultures may be obtained to confirm diagnosis. Treatment includes oral antibiotics or intravenous antibiotics for severe cases. [1]
B) Deep Vein Thrombosis (DVT) refers to the presence of thrombus within a deep vein of the body, most frequently in the lower extremities. [2] Patients are often asymptomatic, but physical exam findings may reveal dilated superficial veins, edema, erythema, and pain or tenderness along the course of the involved major veins. [3] Confirmatory testing is almost always required to ensure proper treatment and prevent complications of inappropriate anticoagulation. The standard treatment for acute DVT is systemic anticoagulation. [2]
C) Hereditary Hemorrhagic Telangiectasia (HHT), also called Osler-Weber-Rendu Syndrome, is a vascular disorder inherited as an autosomal dominant trait. Although a variety of clinical manifestations can occur, the most common manifestations are epistaxis, gastrointestinal bleeding, and iron deficiency anemia, along with characteristic mucocutaneous telangiectasia. A telangiectasia is a small, dilated blood vessel that is visible near the surface of skin or mucous membranes. Management of HHT includes treatment of specific vascular lesions and screening of asymptomatic individuals for arteriovenous malformations (AVMs). [4]
D) Stasis Dermatitis is an eczematous eruption of the lower legs secondary to peripheral venous disease. Clinical manifestations can include varicose veins, pitting edema of the lower legs, brown hyperpigmentation of the involved skin, dull erythema, petechiae, and scaling. If symptomatic, it is usually more itchy than painful. Management of stasis dermatitis is for prevention of venous stasis and edema and includes compression stocking, leg elevation, topical steroids, and wet compresses if oozing or crusting is present. [1]
Varicose Veins
Anisha Mittal, BA; Alexandra Flamm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD; Matthew F. Helm, MD
A 50-year-old female presents with intermittent pain and swelling of the bilateral lower legs which has been occurring for the last 5-6 years. The patient describes the pain as a feeling of pressure and slight burning in her legs, mostly occurring after long periods of standing, walking, or during menstruation. Her pain is relieved by sitting, elevating legs, or wearing compression stockings. Her past medical history includes open-heart surgery for mitral valve prolapse. Patient says her older sister has similar symptoms in her legs. Physical exam reveals dilated veins and mild swelling in the legs, but rest of the skin is unremarkable. The diagnosis of varicose veins is based on both the patient’s history and physical exam findings. The patient is recommended to use compression therapy and leg elevation to manage symptoms.
Varicose veins are a visible manifestation of lower extremity chronic venous disease. They are dilated, elongated, tortuous, subcutaneous veins that are greater than 3 mm in diameter and thought to be more common in women than men. The appearance and visibility of varicose veins is a common concern for patients. Patients may be asymptomatic or symptomatic. Diagnosis of chronic venous disease is based on the presence of typical symptoms such as lower extremity pain, fatigue, heaviness, edema, skin changes, and nonhealing wounds and physical exam findings which reveal visibly dilated superficial veins. Symptomatic patients are often recommended venous duplex ultrasonography to evaluate the nature and extent of venous reflux, which impacts treatment choice. Management of chronic venous disorders is based on clinical severity and level of underlying venous reflux. Patients may opt to undergo treatments such as sclerotherapy, endovenous ablation, venectomy or surface laser. Initial treatment for symptomatic patients includes nonoperative approaches such as skin care, leg elevation, exercise, and compression therapy. Patients who exhibit venous reflux may be candidates for superficial venous ablation via one of many techniques. [5]
References:
1. Marks JG, Miller JJ. Lookingbill and Marks' Principles of Dermatology. 6th ed. Elsevier; 2019.
2. Min SK, Kim YH, Joh JH, et al. Diagnosis and Treatment of Lower Extremity Deep Vein Thrombosis: Korean Practice Guidelines. Vasc Specialist Int. 2016;32(3):77-104. doi:10.5758/vsi.2016.32.3.77
3. Bauer KA. Clinical presentation and diagnosis of the nonpregnant adult with suspected deep vein thrombosis of the lower extremity. UpToDate. Published October 2020.
4. Shovlin CL. Clinical manifestations and diagnosis of hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu syndrome). UpToDate. Published October 2020.
5. Kabnick LS, Sherry Scovell. Overview of lower extremity chronic venous disease. UpToDate. Published October 2020.

A 50-year-old male with a history of anxiety, hepatitis B virus (HBV), which is fully treated, and heroin usage presents to clinic with worsening blisters on his lower legs, arms, and mid-back. Multiple bullae, hyperpigmented scarring, and crusted lesions were found on the patient’s lower extremities. Purple papules were found on the wrists and the mid-back. White striae were found on buccal mucosa. No erosions were present on the mucous membranes.
The patient states that the spots are itchy and tend to blister. He first noticed these blisters 8 years ago when he was working in the heat. The patient tried prednisone and betamethasone with little to no relief. The prednisone helped at first but then the blisters recurred. The patient also tried UV light treatment which irritated the blisters further. What is the most likely diagnosis?
A) Atopic Dermatitis
B) Bullous systemic lupus erythematosus
C) Lichen Planus Pemphigoides
D) Psoriasis
E) Stasis dermatitis
Correct Answer: B) Lichen Planus Pemphigoides
Incorrect Answers:
A) Atopic Dermatitis is a chronic pruritic inflammatory skin disease that often occurs in the pediatric population. Atopic dermatitis is often associated with elevated serum level of immunoglobulin E and a past medical history or family history of atopy. Common features of atopic dermatitis include dry skin and severe pruritus. However, clinical presentation can be variable and characterized by pruritic erythematous papules with exudation and crusting and cutaneous hyperreactivity to environmental stimuli. Management includes topical therapies and wet wraps as first-line approaches and phototherapy, immunosuppressive agents, and methotrexate. [1]
B) Bullous systemic lupus erythematosus is a rare autoimmune blistering disorder that typically manifests as an acute vesiculobullous eruption in patients diagnosed with systemic lupus erythematosus (SLE). Because the differential diagnosis of blistering in patients with SLE is broad, careful assessment is necessary to confirm a diagnosis. Clinical manifestations of this disorder result from the disruption of epidermal-dermal adhesion secondary to antibody formation against Type VII collagen. Treatment recommendations are limited and mainly derived from case reports. [2]
D) Psoriasis is a common chronic inflammatory skin disease that can manifest in many ways. Psoriasis is characterized by well-demarcated, erythematous plaques with overlying, coarse scale. The scalp, extensor elbows, knees, and gluteal cleft are common sites of involvement, and this extent of involvement can range from localized disease to involving most of the body surface area. [2]
E) Stasis dermatitis is a common inflammatory dermatosis of the lower extremities, often occurring in patients with chronic venous insufficiency. Skin findings associated with stasis dermatitis include edema, hyperpigmentation, eczema, fibrosis, atrophy, and ulceration. Hyperkeratosis, parakeratosis, acanthosis, and mild spongiosis are epidermal changes usually observed in stasis dermatitis. Stasis dermatitis also presents with scaling, erythematous, and occasionally pruritus. Treatments target skin dryness, pruritus, inflammation, prevention of ulceration. Patient education is encouraged. [3]
Lichen Planus Pemphigoides
Madison Kist, BS; Matthew F. Helm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD; Alexandra Flamm, MD
A 50-year-old male with a history of anxiety, HBV (which is fully treated), and heroin usage presents to clinic with worsening blisters on his lower legs, arms, and mid-back. Multiple bullae, hyperpigmented scarring, and crusted lesions were found on the patient’s lower extremities. Purple papules were found on the wrists and the mid-back. White striae were found on buccal mucosa. No erosions were present on the mucous membranes. The patient states that the spots are itchy and tend to blister. He first noticed these blisters 8 years ago when he was working in the heat. The patient is recommended to initiate prednisone taper, use a triamcinolone ointment, possibly change hydrochlorothiazide medication and stop UV light treatment, and return to clinic for follow-up. The patient is doing well off of systemic therapy and using the triamcinolone and has experienced occasional flare-ups over the last two years.
Lichen planus pemphigoides (LPP) is a rare autoimmune sub-epidermal blistering disease associated with lichenoid skin changes. [4] A key feature of LPP is the formation of autoantibodies against Type XVII collagen (COL17). In a majority of cases, the COL17-specific autoantibodies in LPP react with the membrane-proximal NC16A subdomain with the C-terminal portion of COL17 and desmoglein 1 as epitopes and antigens. [4] COL17 is a common autoantigen in many autoimmune blistering dermatoses. This development of COL17-specific autoantibodies is suggested to be linked to T cell-mediated lichenoid inflammation in LPP. [4] The diagnosis of lichen planus pemphigoides is dependent on careful correlation between the clinical, histological, and immunological features of the disease. [4] The detection of autoantibodies is critical to securing an LPP diagnosis. Clinical manifestations of the disease include lichenoid papules/plaques and tense blisters. LPP blisters are typically found outside of LP legions and tend to occur on urticated plaques that may evolve into erosions and crusts. LPP lesions are mainly found on the extremities, but can be limited to mucous membranes as well as the nail apparatus, suggesting LPP is a heterogenous disease. Blisters and erosions typically appear after the development of the lichenoid skin changes and classically on previously unaffected skin. [4] Treatment includes topical corticosteroids, intralesional corticosteroids, systemic glucocorticoids, phototherapy, oral retinoids, and oral antihistamines.
References:
1. Schmitt J, Langan S, Deckert S, et al. Assessment of clinical signs of atopic dermatitis: a systematic review and recommendation. J Allergy Clin Immunol 2013; 132:1337.
2. Bolognia J, Schaffer J, Cerroni L. Dermatology. 4th ed. Philadelphia: Elsevier Saunders; 2018.
3. Sundaresan S, Migden MR, Silapunt S. Stasis Dermatitis: Pathophysiology, Evaluation, and Management. Am J Clin Dermatol 2017; 18:383.
4. Hübner, F., Langan, E. A., & Recke, A. (2019). Lichen Planus Pemphigoides: From Lichenoid Inflammation to Autoantibody-Mediated Blistering. Frontiers in immunology, 10, 1389.
Image Challenge: Week 33 - Friday, November 20, 2020

A 51-year-old female presents to the clinic with diffuse firm nodules on her bilateral arms and buttocks areas which began in 2015. She notes that when it originally began, she felt very ill, weak, and fatigued. She was diagnosed with chronic Lyme disease at the time and was treated accordingly. Her treatment was also supplemented with Cat’s Claw, which she still takes today. However, the rash persisted and slowly progressed over time to involve most of her upper arm and upper buttocks. Although it is no longer spreading, the patient reports it to be very painful, which makes it difficult for her to sit. Despite regular dressing changes and follow up appointments with a local wound care clinic every 6 weeks to review dressing change strategies, she reports no symptom improvement. She is unsure of the dose but notes she has been taking daily vitamin D supplements for many years. She denies history of chronic kidney disease. What is the most likely diagnosis?
A) Calcinosis cutis in dermatomyositis
B) Calciphylaxis
C) Chronic tophaceous gout
D) Lupus panniculitis
E) Sporotrichosis
Correct Answer: A) Calcinosis cutis in dermatomyositis
Incorrect Answers:
B) Calciphylaxis is a condition that leads to the calcification of the microvasculature in the dermis and subcutaneous adipose tissue. Although it is common in patients with end stage renal disease, it also can be caused by other conditions that increase serum levels of calcium and phosphate such as a connective tissue disease, secondary hyperparathyroidism, and malignancy. Calcification of the microvasculature can lead to necrosis of the tissue it innervates and can subsequently result in ulcers and poor healing wounds. [1]
C) Chronic tophaceous gout is a chronic form of gout where the urate crystals in a joint have aggregated to form masses called tophi. These tophi can lead to persistent soreness and inflammation. Tophi can present as firm papules over joints that may occasionally ulcerate or drain but are usually not tender themselves. [1]
D) Lupus panniculitis, also referred to as lupus profundus, is an autoimmune condition that presents in individuals both with and without systemic lupus erythematosus. It manifests as firm subcutaneous nodules that are typically seen on the scalp, extremities, and trunk. Ulcerations and calcifications can occur at the site, followed by eventual lipoatrophy. These nodules are not typically painful or present on the buttocks. [1]
E) Sporotrichosis, also referred to as “rose gardener’s disease”, is an infection caused by the dimorphic fungi Sporothrix schenckii. It is typically acquired when activities such as gardening, farming, and agricultural work result in an inoculation of contaminated soil into the skin. Sporotrichosis most commonly presents in its cutaneous form as firm papules along the lymphatics of the arm that can occasionally ulcerate. [2]
Calcinosis Cutis in Dermatomyositis
Radhika Sood, BS; Matthew F. Helm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD; Alexandra Flamm, MD
A 51-year-old female presents to clinic with a rash that presents as diffuse firm nodules on her bilateral arms and buttocks areas with onset in 2015. Notes that when it originally began, she was very ill, weak, and fatigued. She was diagnosed with chronic Lyme disease at the time and treated as such and with a chronic herbal medication. However, the rash persisted and slowly progressed over time to involve most of her upper arm and upper buttocks. Although it is no longer spreading, the patient reports it is very painful and makes it difficult for her to sit. Despite regular dressing changes and follow up appointments with a local wound care clinic every 6 weeks to review dressing change strategies, she reports no symptom improvement. She is unsure of the dose, but has been taking daily vitamin D supplements for many years. She denies a history of chronic kidney disease. The diagnosis of calcinosis cutis in dermatomyositis is made clinically with the patient history, physical exam, a biopsy of one of the lesions on her arms, a muscle biopsy, and serology testing. The arm biopsy confirmed calcinosis cutis. The muscle biopsy showed focal myofiber atrophy indicative of dermatomyositis. The serology testing was positive for ANA and other myositis specific antibodies. The patient was started on IVIG infusions every four weeks and Alendronate 70mg PO every week and recommended to follow up in three months.
Calcinosis cutis is a chronic condition that results in insoluble calcium deposits in cutaneous and subcutaneous tissues. It is commonly associated with autoimmune connective tissue diseases like dermatomyositis. [3] Dermatomyositis is an autoimmune condition that results in progressive muscle weakness and a distinct rash. It is more common in female adults between their late 40s and early 60s. [1] It is suspected that following chronic damage, calcium stores in the mitochondria of myocytes leak out to facilitate the formation of calcium deposits. [3] These can manifest as erythematous and firm nodules that may occasionally ulcerate on the extremities and buttocks. They are often painful and may limit range of motion if they are located above joints. The diagnosis can be made by clinical features, biopsy, and antibody testing. One can also assess the serum levels of calcium, phosphorous, and PTH. [1] There is no definitive treatment, but interventions to help manage the symptoms can be pursued. Medications can be prescribed that target the underlying disease, decrease calcification, and/or reduce inflammation. Depending on the severity, calcium deposits can also be surgically removed. [3]
References:
1. Ward, D. & Fernandez, K. Calcinosis cutis: Etiology and patient evaluation. UpToDate. 2020. Retrieved November 5, 2020, from https://www.uptodate.com/contents/calcinosis-cutis-etiology-and-patient-evaluation/
2. Barros MB, de Almeida Paes R, Schubach AO. Sporothrix schenckii and Sporotrichosis. Clin Microbiol Rev. 2011 Oct;24(4):633-54. doi: 10.1128/CMR.00007-11. PMID: 21976602; PMCID: PMC3194828.
3. Gutierrez A Jr, Wetter DA. Calcinosis cutis in autoimmune connective tissue diseases. Dermatol Ther. 2012 Mar-Apr;25(2):195-206. doi: 10.1111/j.1529-8019.2012.01492.x. PMID: 22741938.
Image Challenge: Week 32 - Friday, November 13, 2020

A healthy 25-year-old female presents to clinic for an evaluation of a brown spot that she had for as long as she can remember. She also reports the color has not changed appreciably over time. According to her parents, she was born with it and it has gotten bigger as she grew-up. There were no other atypical lesions found at birth and no new lesion since. Up to date, she denies any pruritus, drainage, irritation, hair growth, or other changes in the lesion. Physical exam is remarkable only for one sharply demarcated 2 x 4 cm hyperpigmented oval patch on her lower right lumbar region of the abdomen. What is the most likely diagnosis?
A) Becker’s Nevus
B) Café au Lait Macule
C) Congenital Melanocytic Nevus
D) Congenital Melanocytosis
E) Lentigo Simplex
Correct Answer: B) Café au Lait Macule
Incorrect Answers:
A) Becker’s melanosis is a hamartoma that presents as patchy hyperpigmentation with various degrees of hypertrichosis. It is typically found in the upper lateral trunk with irregular borders. Becker’s nevi are much more common in males. Hyperpigmentation appears in the first decade of life with the hypertrichosis, if any, appearing in the second. [1]
C) Congenital melanocytic nevi (CMN) are a proliferation of benign melanocytes that are often present at birth or arise soon after birth. A solitary 2 x 4cm patch, as presented in the case, is unlikely to be a CMN because as an adult, CMN typically appear as plaques with a mammilated or cobblestone texture and prominent terminal hairs. CMN are classified based on their size. Small CMN are <1.5 cm, medium being 1.5-19.9 cm, and large being >20cm. Small and medium CMN have a 2-5% risk of malignant transformation into melanoma and should be monitored for changes. Large CMN have a higher risk, between 6-20%, that prompts an immediate referral to a specialist. [1]
D) A lentigo simplex is a hyperpigmented macule that presents in childhood. They are usually smaller than 5 mm in size and are typically well-demarcated, round or oval, and can appear on any area of the body, including mucus membranes, genitalia, and conjunctiva. Simple lentigines in certain distributions can be due to an underlying syndrome, such as Peutz-Jeghers. The more common type of lentigo is actinic/solar, colloquially known as liver or age spots. Actinic lentigines commonly appear later in life on sun exposed skin. [1]
E) Congenital melanocytosis, previously referred to as “Mongolian spots” are blue-gray patches of dermal melanocytosis commonly found in the lumbosacral region. They present at birth and are common in Asian, African American, and Native American people. Regression typically occurs within early childhood, but lesions that occur outside of the lumbosacral area tend to linger longer throughout life. [1]
Café au Lait Macule
Ramon Govea, BS; Matthew F. Helm, MD; Alexandra Flamm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD
A healthy 25-year-old female presents to clinic for an evaluation of a brown spot that she had for as long as she can remember. She also reports the color has not changed appreciably over time. According to her parents, she was born with it and it has gotten bigger as she grew-up. There were no other atypical lesions found at birth and no new lesion since. Up to date, she denies any pruritus, drainage, irritation, hair growth, or other changes in the lesion. Physical exam is remarkable only for one sharply demarcated 2 x 4 cm hyperpigmented oval patch on her lower right lumbar region of the abdomen. The diagnosis of a benign café au lait birthmark was made. The patient was reassured that there were no red flags and no indications for further intervention.
Café au lait spots (CALS) are congenital, well demarcated macules and patches that become more clinically apparent early in life due to increasing melanogenesis within the lesions. One or more CALS can be found on exam. Small and solitary CALS are typically benign and require no further investigation. Multiple or large CALS can expand the differential diagnosis. Neurofibromatosis type 1 (NF1) and McCune Albright’ Syndrome (MAS) are two examples where CALS are common. Early in childhood, NF1 will present with multiple CALS as well as other cutaneous manifestations such as inguinal and axillary freckling, Lisch nodules in the eyes, and neurofibromas. The CALS in MAS are characterized with sharp demarcation at the midline of the trunk. When such morphologies and distributions of CALS occur, further work up and appropriate consultation of other specialties are required. Fortunately, there have been no reports of CALS undergoing malignant changes. CALS themselves do not need to be treated, but underlying syndromes associated with CALS, if present, should. [1]
Reference:
1. Bolognia J, Schaffer J, Cerroni L. Dermatology. 4th ed. Philadelphia: Elsevier Saunders; 2018.

A 57-year-old female with a family history of systemic lupus erythematosus presents to clinic with a “rash” that has been present for three months. She first noticed the rash on her bilateral forearms, which has since spread to her legs, back, and face. The rash consists of hypopigmented patches and is pruritic. She has also noticed symmetric thickening of the skin. She endorses new onset reflux and difficulty swallowing solid food. Her fingers also turn colors and become painful when she is outside in the cold. Physical exam reveals periungual telangiectasias. She has never experienced anything like this before and takes no medications. What is the most likely diagnosis?
A) Eosinophilic Fasciitis
B) Lichen Sclerosis
C) POEMS Syndrome
D) Primary Amyloidosis
E) Scleroderma
Correct Answer: E) Scleroderma
Incorrect Answers:
A) Eosinophilic Fasciitis – Eosinophilic fasciitis is a rare condition that begins as trunk and limb erythema, which can progress to thickening of the subcutaneous fascia over time. A variety of other symptoms can be present, such as arthralgias, myalgias, and neuropathies. However, with the exception of rare cases, there is no visceral organ involvement or presence of Raynaud’s phenomenon. Sclerosis is usually asymmetric in nature. It is thought that it could be induced by exercise, but the pathogenesis of this condition is poorly understood. [1]
B) Lichen Sclerosis - Lichen sclerosis is a chronic inflammatory condition that results in white, atrophic plagues on the skin. The exact pathogenesis is not well understood, although it is believed that trauma, antibodies to ECM-1, and genetic predisposition plays a pivotal role. Typically, these lesions are pruritic and found on female genitalia, but can also be extragenital. Lichen Sclerosis also carries an increased risk of developing squamous cell carcinoma in involved areas. [2]
C) POEMS Syndrome – POEMS syndrome is a neoplastic syndrome that is characterized by polyneuropathy, organomegaly, endocrinopathy, M-protein, and skin changes. Skin changes can be seen in this condition, most commonly sclerodactyly, pigmentary changes, and glomeruloid hemangiomas. One of the criteria required for diagnosis is the presence of a subacute demyelinating neuropathy. Elevated VEGF is highly specific for POEMS Syndrome, and is believed to be related to the pathogenesis, which is not fully understood [3].
D) Primary Amyloidosis- Amyloidosis is caused by the deposition of an insoluble protein (there are many different types of protein that can cause it) in certain locations of the body. Primary amyloidosis is due to deposition of amyloid light chain in a variety of organs, such as kidney, liver, heart, nerves, GI tract, and skin. It is typically secondary to a primary plasma cell dyscrasia, such as multiple myeloma. Diagnosis is usually confirmed with punch biopsy of the affected area of skin and stained with Congo red stain. Treatment is directed at treating the underlying dyscrasia to reduce the production of the monoclonal light chain. [4]
Scleroderma
Ty J. Achtermann, BS; Alexandra Flamm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD; Matthew F. Helm, MD
A 57-year-old healthy female presents to clinic with a rash that has been present for three months. She first noticed the rash on her bilateral forearms, which has since spread to her legs, back, and face. The rash is pruritic, has hypopigmented patches, and never subsides. She feels that her skin has become thicker where the rash is present. She is suffering from new onset reflux and difficulty swallowing solid food. Her fingers turn colors and become painful when she is outside in the cold and has periungual telangiectasias. She has also experienced a 30-pound weight loss over the past few months. A punch biopsy of the rash revealed sclerotic collagen bundles and a sparse lymphoplasmacytic infiltrate. ANA titers were positive at 1:2560 with a speckled pattern. The results of the biopsy and ANA titers, as well as her skin thickening, Raynaud phenomenon, periungual telangiectasias, acid reflux, and difficulty swallowing food is sufficient to diagnose scleroderma in this patient. The patient will be started on a prednisone taper and mycophenolate mofetil. In order to rule out involvement of other organs, pulmonary function tests and a urinalysis will be performed. Physical therapy and exercise are encouraged to reduce the likelihood of joint contractures.
Systemic sclerosis, or scleroderma, is a chronic, progressive condition that results in fibrosis of the skin as well as internal organs. It is proposed that the mechanism of fibrosis is due to overproduction of extracellular matrix by activated fibroblasts, from a complex interaction of lymphocytes, macrophages, and cytokines, and growth factors. [5] The exact incidence of this disease is difficult to report, although estimates are between 8 to 56 new cases per million persons each year. [6] Symmetric fibrosis of the skin is most universal finding among patients with scleroderma, but many other organ systems are often affected, such as musculoskeletal, gastrointestinal, pulmonary, cardiac, renal, neuromuscular, and genitourinary. Skin thickening from the fingers extending proximal to the MCPs are characteristic. Depending on the extent and severity of organ involvement, scleroderma will further be classified into a subtype. The most common subtypes consist of limited cutaneous systemic sclerosis, diffuse cutaneous sclerosis, systemic sclerosis sine scleroderma, and systemic scleroderma with overlap syndrome, although overlap between subtypes can occur. Confirming a diagnosis of scleroderma can be difficult, as it often overlaps with other connective tissue disorders. A diagnosis is typically made with physical exam findings of skin thickening combined with other signs of systemic fibrosis. Antibody testing for anti-scl-70, ACA, anti-RNA polymerase III, and ANA may be useful. A biopsy of affected skin showing sclerotic collagen bundles can help confirm a diagnosis. Treatment in an individual with extensive organ involvement is with immunosuppressive therapy. Mycophenolate, methotrexate, cyclosporine, and other immunosuppressive agents are used. [7,8] Treatment also usually consists of symptom management. For example, a proton pump inhibitor may be prescribed in a patient with GERD from esophageal sclerosis.
References:
1. Chanda JJ, Callen JP, Taylor WB. Diffuse fasciitis with eosinophilia. Arch Dermatol. 1978 Oct;114(10):1522-4. PMID: 718192.
2. Powell JJ, Wojnarowska F. Lichen Sclerosus. The Lancet. 1999 May;353(9166):1777-1783. https://doi.org/10.1016/S0140-6737(98)08228-2
3. Brown R, Ginsberg L. POEMS syndrome: clinical update. J Neurol. 2019;266(1):268-277. doi:10.1007/s00415-018-9110-6
4. Chang A.Y. (2018) Systemic Amyloidosis. In: Rosenbach M., Wanat K., Micheletti R., Taylor L. (eds) Inpatient Dermatology. Springer, Cham. https://doi.org/10.1007/978-3-319-18449-4_75
5. Yamamoto T. Scleroderma--pathophysiology. Eur J Dermatol. 2009 Jan-Feb;19(1):14-24. doi: 10.1684/ejd.2008.0570. Epub 2008 Dec 5. PMID: 19059831.
6. Ingegnoli F, Ughi N, Mihai C. Update on the epidemiology, risk factors, and disease outcomes of systemic sclerosis. Best Pract Res Clin Rheumatol. 2018 Apr;32(2):223-240. doi: 10.1016/j.berh.2018.08.005. Epub 2018 Sep 14. PMID: 30527428.
7. Nihtyanova SI, Brough GM, Black CM, Denton CP. Mycophenolate mofetil in diffuse cutaneous systemic sclerosis--a retrospective analysis. Rheumatology (Oxford). 2007 Mar;46(3):442-5. doi: 10.1093/rheumatology/kel244. Epub 2006 Aug 9. PMID: 16899504.
8. Appelboom T, Itzkowitch D. Cyclosporine in successful control of rapidly progressive scleroderma. Am J Med. 1987 Apr;82(4):866-7. doi: 10.1016/0002-9343(87)90046-5. PMID: 3565449.
Image Challenge: Week 31 - Friday, November 6, 2020

A 20-year-old otherwise healthy female presents to the dermatology clinic with complaints of a red, slightly pruritic rash on her right lateral thigh that has been present for two weeks. She has had similar rashes in the past five years that typically occur in the fall and winter and affect her legs and arms. Lesions often occur in groups and will start as red, circular patches that later develop a central clearing. She has tried non-medicated lotion with minimal relief and lesions typically go away on their own after approximately one month. She has noticed an increase in rash frequently since moving from Georgia to New York. A KOH preparation in the past was negative. She denies any known allergies or associated illness. She is a college athlete and denies any contacts with a similar rash. What is the most likely diagnosis?
A) Allergic contact dermatitis
B) Annular lichen planus
C) Erythema annulare centrifugum
D) Nummular eczema
E) Tinea corporis
Correct Answer: D) Nummular eczema
Incorrect Answers:
A) Allergic contact dermatitis is an inflammatory reaction of the skin in response to an exogenous chemical typically 24-48 hours after exposure. Lesions can range from vesicles to eczematous reactions that can become chronic and show changes such as lichenification. The shape of the lesion depends on the nature of the exposure which may result in patches or plaques with geometric outlines and sharp margins. [1]
B) Annular lichen planus is a rare morphological variant of lichen planus, an inflammatory skin condition. Lesions are most commonly found on genitals and intertriginous zones, but also can occur on the lips, trunks, or arms. They present as red to purple circular macules or papules with raised borders with or without central atrophy. Annular lichen planus has a male predominance and is often asymptomatic. [2]
C) Erythema annulare centrifugum is characterized by waxing and waning annular red plaques that expand centrifugally and have a characteristic trailing edge of scale inside the elevated border. Lesions are chronic and can recur up to several years. The location most commonly involves the axilla, hips, and thighs. The cause is unknown, and treatment is often unhelpful. [1]
E) Tinea Corporis is a fungal skin infection. The typical presentation is an annular lesion with an elevated, erythematous patch with a scaling, serpiginous, or worm-like border and tendency for central clearing. Multiple lesions may be present at once. KOH examination will demonstrate hyphae. Incidence is higher in warmer, more humid climates. [1]
Nummular Eczema
Catherine Smiley, BA; Matthew F. Helm, MD; Alexandra Flamm, MD; Joslyn Sciacca Kirby, MD; Brian Green, DO
A 20-year-old otherwise healthy female presents to the dermatology clinic with complaints of a red, slightly pruritic rash on her right lateral thigh that has been present for two weeks. She has had similar rashes in the past five years that typically occur in the fall and winter and affect her legs and arms. Lesions often occur in multiples and will start as red, circular patches that later develop a central clearing. She has tried non-medicated lotion with minimal relief and lesions typically go away on their own after approximately one month. She has noticed an increase in rash frequently since moving from Georgia to New York. A KOH preparation in the past was negative. She denies any known allergies or associated illness. She is a college athlete and denies any contacts with a similar rash. Physical exam demonstrates a 16mm, well-circumscribed, red, annular patch with central clearing and peripheral scale. A KOH is completed that does not demonstrate any evidence of hyphae and a diagnosis of nummular eczema is made. The patient is prescribed hydrocortisone 2.5% cream and develops resolution of rash with daily application after two weeks. Subsequent lesions resolve quicker with this treatment regimen.
Nummular eczema is a type of essential dermatitis that affects men more often than women. Most patients are over the age of 50, although individuals of any age can be affected. [1,3] The lesions of nummular eczema are typically multiple and characterized by coin-shaped, pruritic, weeping patches with crusted papulovesicles. [1] After an acute phase, nummular eczema may progress to a scaly stage with central clearing and peripheral extension, causing ring-shaped lesions. [4] It presents most frequently on the hands, arms, and legs. The rash develops during cold, dry months. Nummular eczema is commonly mistaken as tinea corporis and can be distinguished with a negative KOH preparation. Histologic findings demonstrate intercellular edema causing spongiosis. Corticosteroid therapy is the first-line treatment for nummular eczema and can be used topically, intralesionally, or systemically depending on the severity of symptoms. [1]
References:
1. Marks JG, Jr, Miller JJ, Lookingbill DP, Marks JG, Jr. Lookingbill and Marks' Prinicples of Dermatology. Sixth ed. Place of publication not identified: ELSEVIER; 2018.
2. Weston G, Payette M. Update on lichen planus and its clinical variants. Int J Womens Dermatol. 2015;1(3):140-149. Published 2015 Sep 16. doi:10.1016/j.ijwd.2015.04.001
3. Susan Burgin. Nummular eczema, lichen simplex chronicus, and prurigo nodularis. In: Fitzpatrick's Dermatology in General Medicine, 8th ed, Goldsmith LA, Katz SI, Gilchrest BA, et al (Eds), McGraw-Hill, 2012. Vol 1, p.182.
4. Narayanasetty NK, Pai V V., Athanikar SB. Annular lesions in dermatology. Indian J Dermatol. 2013. doi:10.4103/0019-5154.108071
Image Challenge: Week 30 - Friday, October 30, 2020

A 76-year-old male with a past medical history of rheumatoid arthritis presented with a 1-month history of a worsening rash on both of his palms. The rash was causing burning and pruritis. Four days ago, he had stopped oral steroids that helped with the rash. He was treating it with only an over-the-counter moisturizer, which was not helping the rash. He denied any recent illnesses and had not had any new medications in the six months prior to the rash. He had never smoked and did not have any history of other skin conditions. Upon review of systems he denied joint pain or swelling, fevers, eye pain, vision changes, dysuria, abdominal pain, diarrhea, and leg pain or swelling. On physical examination, erythematous plaques with scales were noted bilaterally on his palms. The rest of the skin exam was unremarkable with no evidence of cutaneous plaques or scales. Which of the following is the most likely diagnosis?
A) Cutaneous candidiasis
B) Dermatitis herpetiformis
C) Hand-foot-mouth disease
D) Keratoderma blenorrhagicum
E) Palmoplantar pustulosis
Correct Answer: E) Palmoplantar pustulosis
Incorrect Answers:
A) Candida is an opportunistic pathogen that causes cutaneous and mucosal infections with the potential to produce disseminated disease. Cutaneous candidiasis is characterized by the classic triad of fever, myalgia, and rash. The rash of a localized Candida infection commonly presents as beefy-red plaques with satellite papules and pustules. The rash is often found in moist areas, such as the diaper area, axillae, or groin folds. Risk factors for infection include extremities of age, pregnancy, and use of corticosteroids or immunosuppressive medications. Cutaneous candidiasis can be confirmed with bedside potassium hydroxide (KOH) preparation. The treatment regimen of cutaneous candidiasis consists of topical imidazoles, such as ketoconazole, and in severe cases oral antifungals, such as fluconazole, are used. [1]
B) Dermatitis herpetiformis (DH) is an autoimmune disorder that classically presents with a symmetric distribution of pruritic and burning erythematous vesicles, which may be disrupted by scratching, such that erythematous erosions are seen on exam. The primary lesions may be purpura when they occur on the palm, papules, or crusts. The distribution includes the extensor surfaces of the arms and legs, buttocks, scalp, and face. Patients with DH have higher incidences of other autoimmune diseases such as celiac disease and lupus erythematosus. Gluten plays a role in creating the proinflammatory skin environment that leads to the development of these skin lesions. Direct immunofluorescence shows granular dermal papillary deposits of IgA. On histology, skin lesions are characterized by dermal papillary collections of eosinophils, neutrophils, and subepidermal vesiculation. [1]
C) Hand-foot-mouth disease (HFMD) is most commonly seen in children in the summer and fall seasons. It is most commonly caused by coxsackievirus and enteroviruses via the fecal-oral route of transmission, with an incubation period of 3-6 days. Typical HFMD presents with fever, malaise, upper respiratory tract symptoms, and diarrhea in children. The hallmark of HFMD is vesicular lesions found on the palms, soles, buttocks, and tongue that progress from pink macules and papules to vesicles with a base of erythema. These vesicles erode and form gray “football-shaped” lesions with an erythematous halo, lasting 7-10 days. In typical HFMD, infected adults rarely show signs of infection, whereas in atypical HFMD, adults may present with diffuse involvement with exanthem. Treatment aims to reduce dehydration and discomfort. [1]
D) Keratoderma blenorrhagicum is one of the cutaneous manifestations of reactive arthritis. This syndrome can include urethritis, conjunctivitis (or keratitis or iritis), and arthritis. Few people develop all of the findings. The syndrome often occurs in young men following a bout of urethritis or diarrheal illness. People can also develop a rash, reminiscent of psoriasis, on the palms, soles, and genitals. Keratoderma blenorrhagicum is the term that describes the erythematous vesicular lesion that progresses into pustular keratotic lesions, which then coalesce into psoriatic-like plaques. It is treated with topical corticosteroids, phototherapy, keratolytics, and oral methotrexate for severe cases. [1]
Palmoplantar Pustulosis (PPP)
Rucha Borkhetaria, BS; Matthew F. Helm, MD; Alexandra Flamm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD
A 76-year-old male with a past medical history of rheumatoid arthritis presented with a 1-month history of a worsening rash on both of his palms. The rash was causing burning and pruritis. Four days ago, he had stopped oral steroids that helped with the rash. He was treating it with only an over-the-counter moisturizer, which was not helping the rash. He denied any recent illnesses and had not had any new medications in the six months prior to the rash. He had never smoked and did not have any history of other skin conditions. Upon review of systems he denied joint pain or swelling, fevers, eye pain, vision changes, dysuria, abdominal pain, diarrhea, and leg pain or swelling. On physical examination, erythematous plaques with scales were noted bilaterally on his palms. The rest of the skin exam was unremarkable with no evidence of cutaneous plaques or scales. Based on his history and exam, palmoplantar pustulosis was diagnosed. His initial treatment regimen consisted of topical 0.05% clobetasol cream 1-2 times daily for 7-10 days, and topical 0.005% calcipotriene daily, and was advised to expose his hands to ambient light.
Palmoplantar pustulosis (PPP) is a rare localized variant of pustular psoriasis and presents with recurring pustular eruptions of the palms and soles. Crops of 2 to 4mm pustules arise on palmar and plantar skin, that turn from yellow to brown over time. These eruptions rarely extend to the feet, volar wrists, or dorsa of the fingers, and are sometimes accompanied by pruritis and burning. On histology, sterile intraepidermal pustules with polymorphonuclear leukocytes, with surrounding spongiform changes, are seen. PPP follows a chronic course, and remissions may last a few months. PPP is more common in females, with onset between the ages of 20 and 60 years. While the cause of PPP is unknown, the proposed mechanism of pustule formation is decreased skin-derived antileukoprotease (elafin) activity. Smoking, tonsillitis, humidity, and high temperatures are strongly associated with PPP. Treatment includes topical corticosteroids and calcipotriene, which are often combined with colchicine (0.6mg twice a day) or acitretin (25 to 50 mg/daily orally). [2]
References:
1. Bruckner AL. Fitzpatrick's Dermatology. 9th ed. McGraw-Hill: 2019.
2. Mengesha YM, Bennett ML. Pustular skin disorders: diagnosis and treatment. Am J Clin Dermatol. 2002; 3(6):389-400.

A 26-year-old male presents to the clinic with occasionally itchy bumps on neck, chest, back and arms. He first noticed the lesions 4 weeks ago and states they appear more frequently after sweating and staying in his gym clothing for an extended time period. He denies any recent travel, outdoor activities or use of new personal care products. On physical exam, multiple diffuse papules and pustules on an erythematous base across back of neck, chest, upper back and upper arms were observed. He denies any fever or other systemic symptoms. The patient is otherwise healthy with no significant past medical history. No relevant family history. What is the most likely diagnosis?
A) Allergic contact dermatitis
B) Folliculitis
C) Hidradenitis suppurativa
D) Keratosis pilaris
E) Papular urticaria
Correct Answer: B) Folliculitis
Incorrect Answers:
A) Allergic contact dermatitis (ACD) is a T-cell mediated, delayed type IV hypersensitivity reaction of the skin that can cause tissue inflammation. Clinical presentation includes pruritic erythematous, indurated, scaly plaques, and is typically localized to the skin areas that come in contact with the allergen. Chronic ACD may also display lichenification, scaling, and fissuring. [1] Common causes of allergic contact dermatitis include poison ivy or oak, cosmetic or personal care products, nickel, rubber compounds, and topical medications. [2] Delay in reaction, which can be up to 72 hours, can make identifying exposures difficult but a patch test can be used to confirm the diagnosis of ACD. Treatment of ACD includes avoidance of the allergen and topical or systemic corticosteroids depending on severity. [1]
C) Hidradenitis suppurativa (HS) is a chronic inflammatory disorder most commonly located in the axillary, inguinal, and anogenital regions. Clinical presentation generally includes inflamed and noninflamed papules, cyst, or nodules. Secondary lesions of HS including pyogenic granulomas in sinus tract openings and scarring may also be seen. Women are more frequently affected than men, with a female to male ratio of 3:1. [3] The Hurley staging system is used to determine best treatment plan. Mild to moderate disease is often treated with topical antibiotics and local steroid injections. In severe cases of HS, systemic immunosuppressive agents, surgical excisions, and injectable biologic agents are used. [2]
D) Keratosis pilaris is a common condition characterized by keratinized hair follicles that present as individual, small pink/red follicular papules usually on the upper arms, thighs, cheeks, or buttocks. These bumps are generally not painful or pruritic. Patients regularly report “rough bump” that worsens in the winter. Laboratory workup and biopsy are not necessary for diagnosis. Treatment of keratosis pilaris consists of patient education and reassurance, however, an emollient cream containing 20% urea, 6% salicylic acid, and ammonium lactate 12% may be used to soften the rough papules. [2]
E) Papular urticaria is a chronic immunological reaction induced by insect bites, most often fleas, mosquitoes, spiders, or bed bugs. Clinical presentation includes chronic pruritic papules or vesicles on exposed areas of the skin including arms, lower legs, upper back, and scalp. Treatment includes anti-histamines for pruritis and mid-potency topical corticosteroids applied to lesions. [4]
Folliculitis
Meloria Hoskins, MS; Alexandra Flamm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD; Matthew F. Helm, MD
A 26-year-old male presents to the clinic with occasionally itchy bumps on neck, chest, back and arms. He first noticed the lesions 4 weeks ago and states they appear more frequently after sweating and staying in his gym clothing for an extended time period. He denies any recent travel, outdoor activities or use of new personal care products. On physical exam, multiple diffuse papules and pustules on an erythematous base across back of neck, chest, back and upper arms were observed. He denies any fever or other systemic symptoms. The patient is otherwise healthy with no significant past medical history. No relevant family history. Based on his history and exam, the patient was diagnosed with bacterial folliculitis and given clindamycin swabs to use twice a day and as needed after sweating. His folliculitis improved with clindamycin and will follow-up as needed.
Folliculitis refers to inflammation of the hair follicle with the classic clinical findings of follicular pustules and erythematous papules on hair-bearing skin and is often confused with or occurs simultaneously with, acne vulgaris. Conditions that make patients more susceptible to folliculitis include rubbing skin frequently, shaving, hot and humid temperatures, or wearing tight clothing. Pruritis is the most common associated symptom. Nodules may be seen as a feature of deep follicular inflammation. Folliculitis may be infectious or non-infectious. Identification of the type of infection is important because treatment differs for each. Bacterial infection, most often caused by Staphylococcus aureus, is the most common cause of infectious folliculitis. The gram-negative bacteria Pseudomonas aeruginosa can lead to folliculitis due to contact with contaminated water, also known as “hot tub folliculitis.” Folliculitis may also be caused by fungal species or viruses. Multiple species of Malassezia can lead to Pityrosporum folliculitis, which is typically diagnosed in younger male patients due to increased sweating and sebum production. Viral folliculitis is most commonly caused by the herpes virus and presents similarly to bacterial folliculitis with the exception that lesions typically appear in clusters. Patient history, physical examination, and localization of lesions should be used for diagnosis as they may offer clues to the etiology. A Gram stain and culture of contents of a pustule can confirm the presence and identification of an infectious organism. Treatment is not always necessary as mild folliculitis will often resolve on its own, however, patients with papules or pustules on multiple areas of the body may be treated with topical or oral antimicrobials depending on infectious organism present. [2]
References:
1. Nassau S, Fonacier L. Allergic Contact Dermatitis. Medical Clinics of North America. 104 (1) pp. 61-76 (2020).
2. Marks J G, Miller J J. Lookingbill and Marks Principles of Dermatology, 6e. Philadelphia: Elsevier. (2019).
3. Gregor B.E. Jemec. Hidradenitis Suppurativa. N Engl J Med. 366:158-164 (2012)
4. Demain, J.G. Papular urticaria and things that bite in the night. Curr Allergy Asthma Rep 3, 291–303 (2003).

A 17-year-old Asian male presents to clinic with persistent growth on his elbow. He had an abrasion to his elbow 6 months ago, where he scraped it on the turf during a game of football. He reports the injury had minimal bleeding and had not been infected during the healing process. 2 months ago, he noticed a protuberance at the site of the previous abrasion that extended beyond the margins of the original abrasion. He reports mild redness and pain at the injury site during physical activity such as doing push-ups, which resolved approximately 20 mins of stopping physical activity. On physical exam, he has a 2.5cm firm, waxy plaque with a hyperpigmented center. What is the most likely diagnosis?
A) Atrophic scar
B) Dermatofibroma
C) Hypertrophic scar
D) Keloid
E) Lobomycosis
Correct Answer: D) Keloid
Incorrect Answers:
A) Atrophic scars are characterized as flat or depressed skin lesions with an indented center, and can be subclassified into boxcar, icepick, or rolling morphology. These scars are caused by inflammatory mediators and enzymatic damage to the epidermis and dermal collagen. Atrophic scars commonly appear in patients with severe acne vulgaris or after infections from varicella and herpes simplex virus. [1]
B) Dermatofibromas appear as firm papules or nodules with a hypopigmented center and are composed of fibrous tissue. These can vary from 0.5-1.5cm in diameter, and are tethered to the skin surface and mobile over subcutaneous tissue. Their cause is unknown, but are thought to be caused by previous injury to the area. The lesions frequently develop on the lower extremities and are more common in women than men. [2]
C) Hypertrophic scars are characterized as papules or nodules that can be erythematous or pruritic. Unlike keloids, these tend to be less nodular and do not grow beyond the boundary of the injury. Hypertrophic scars are due to an overly aggressive healing process after physical injury to body tissue. These are common after thermal injuries and usually develop within a few weeks after injury to skin. This type of scar can undergo partial spontaneous resolution and improve naturally. [3]
E) Lobomycosis is a fungal infection of the skin caused by Lacazia loboi and appear as keloidal nodular lesions that contain round fungal organisms arranged in a linear “pop-bead” like configuration. Infection commonly develops after minor scratches or insect bites and is endemic in rural regions in South America and Central America. [3]
Keloid
Lisa Ho, BS; Matthew F. Helm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD; Alexandra Flamm, MD
A 17-year-old Asian male presents to clinic with persistent growth on his elbow. He had an abrasion to his elbow 6 months ago, where he scraped it on the turf during a game of football. He reports the injury had minimal bleeding and had not been infected during the healing process. 2 months ago, he noticed a protuberance at the site of the previous abrasion that extended beyond the margins of the original abrasion. He reports mild redness and pain at the injury site during physical activity such as doing push-ups, which resolved approximately 20 mins of stopping physical activity. On physical exam, he has a 2.5cm firm, waxy plaque with a hyperpigmented center. The diagnosis of a keloid is made clinically with patient history and physical exam. The patient was given several intralesional corticosteroid injections over the course of 4 months to help shrink the size of the scar and relieve the associated symptoms.
During normal scar formation, collagen is arranged in discrete fascicles separated by interstitial space. A keloid is a type of raised scar that results from overly aggressive pro-inflammatory mediators such as TNF-alpha, IL-1 alpha, IL-1 beta, and IL-6, causing an increase in collagen growth in a disorganized arrangement. [3] In contrast to hypertrophic scars, keloid scars extend beyond the original injury, and remain red and occasionally painful rather than regressing after a few months. Keloid scars most commonly affect 10-30 year olds. Risk factors for keloid formation include patients of African, Hispanic, or Asian descent, family history, and wounds on chest, shoulders, upper arms, earlobes, or cheeks. [3] The diagnosis of keloids is based on the location, appearance, and progression of the scar over time. There is no universally accepted treatment approach for keloids. Treatment options include silicone sheeting, pressure treatment to reduce fibroblast proliferation, or corticosteroid injections to reduce pain and inflammation. [4] Cryotherapy can be useful for smaller lesions. Surgical removal of keloids usually provides only temporary relief as it can cause more aggressive regrowth of scar tissue. [4]
References:
1. Majid I, Imran S. Fractional CO2 Laser Resurfacing as Monotherapy in the Treatment of Atrophic Facial Acne Scars. J Cutan Aesthet Surg. 2014;7(2):87-92. doi:10.4103/0974-2077.138326
2. Myers DJ, Fillman EP. Dermatofibroma. StatPearls. 2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470538/
3. Goldstein B, Goldstein A, & Hong A. Keloids and hypertrophic scars. In R. Corona (Ed.), UpToDate. 2020. Retrieved October 25, 2020, from https://www-uptodate-com.medjournal.hmc.psu.edu:2200/contents/keloids-and-hypertrophic-scars?search=pathophysiology%20of%20keloid&source=search_result&selectedTitle=1~86&usage_type=default&display_rank=1
4. Juckett G, & Hartman-Adams H. Management of keloids and hypertrophic scars. American family physician. 2009; 80(3), 253–260.
Image Challenge: Week 29 - Friday, October 23, 2020

A 44-year-old female presented to clinic with a several month history of a rash on her left pinky toe and top of the left foot. The rash first appeared after a hospital stay for a hysterectomy and subsequent bladder sling placement. The rash does not cause any itching or discomfort. It is not accompanied by any other symptoms and is not present anywhere else. Which of the following is the likely diagnosis?
A) Annular lichen planus
B) Atopic dermatitis
C) Erythema annulare centrifugum
D) Granuloma annulare
E) Tinea Pedis
Correct Answer: D) Granuloma annulare
Incorrect Answers:
A) Annular lichen planus presents with violaceous, pruritic papules that can affect the skin, mucous membranes, scalp, and genitalia. Clinical manifestations are remembered by the “four Ps”: pruritic, purple, polygonal, and papules/plaques. Upon close inspection, fine white lines can be seen on the surface of the lesions, collectively known as “Wickham’s striae”. First line therapy is topical corticosteroids, for pruritic relief mainly, as the lesions tend to resolve on their own
B) Atopic dermatitis or “eczema” is pruritic inflammatory skin disease most commonly occurring in children but can also affect adults. Acute eczema presents as intensely pruritic erythematous plaques and vesicles with exudate and crusting. Chronic lesions tend to be dry, scaly, or excoriated erythematous papules. Lichenification or skin thickening can occur over time from the repeated trauma from scratching. The pathophysiology is multifactorial involving skin barrier defects, failure of immune regulation, and altered skin microbial flora. Risk factors include a family history of atopy where a genetic predisposition to produce IgE following exposure to certain allergens is increased. Treatment involves removal of the offending allergen, maintaining adequate skin hydration through the use of emollients, and use of topical immunosuppressants.
C) Erythema annulare centrifugum presents with multiple annular, erythematous plaques demonstrating the characteristic rim of scale along the inner margin of the lesion. Although it can occur anywhere on the body, the trunk and lower extremities are most common. Additional symptoms can include swelling and pruritis. Histopathologic findings include dense lymphocytic infiltrate surrounding blood vessels, which distinguishes it from granuloma annulare. Pathogenesis remains unclear and is thought to be due to a delayed hypersensitivity response with literature describing medications, diseases, infections and allergens as potential triggers. Treatment involves removing the offending trigger, and if one cannot be identified, then local corticosteroids can reduce inflammation.
E) Tinea pedis is a cutaneous dermatophyte infection that presents as a pruritic, circular, erythematous, scaling patch/plaque. A central clearing with a raised outer border creates the resulting annular ring-shaped plaque from which the name “ringworm” is derived. Risk factors include contact sports in which skin to skin contact occurs. Diagnosis is performed by KOH preparation demonstrating segmented hyphae characteristic of dermatophytes. Treatment consists of topical antifungals.
Granuloma Annulare
Matthew Bierowski, BS; Alexandra Flamm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD; Matthew F. Helm, MD
A 44-year-old female presents to clinic with chief complaint of a left foot rash that has been present for several months. The patient denies any change in size or additional areas of rash. The patient first noticed the rash after a hysterectomy complicated by placement of a bladder sling. She has not tried any treatment for it as it is not pruritic and does not cause any discomfort. There are no other associated symptoms and she has not started any new medications. On physical exam, there are two ring shaped patches without overlaying scale on the dorsal aspect of the left foot. KOH prep was performed to rule out fungal infection and was negative. Based on history and exam, granuloma annulare was diagnosed. She is treated with 0.05% clobetasol cream on the affected areas twice a day for 2 weeks at a time with at least 1 week off in between weeks.
Granuloma annulare is a self-limiting disorder characterized by the presence of erythematous, non-scaly annular plaques, most commonly arising on the distal extremities. The lesions can present locally, as seen in this case, or can be more diffuse. [1] While the exact pathogenesis remains unknown, there have been cases reported in literature linking granuloma annulare to various diseases, medications, trauma, sun exposures, vaccines, and post infection. Although limited to case reports, there may be a link to malignancy and diabetes and some providers argue to screen for these diseases in those with granuloma annulare. [2,3] Clinically, most patients present complaining of the rash cosmetically, as it is usually asymptomatic. On close examination, the lesion will demonstrate an annular plaque with a rope like border and central clearing. [4] Small papules may be found at the periphery of the main lesion. On histological biopsy, a lymphohistiocytic infiltrate is seen with degeneration of the surrounding collagen and mucin deposition. [5] Although biopsy is the gold standard for diagnosis, it can usually be made clinically. Due to its ability to masquerade as other skin diseases, infectious and other immune mediated skin lesions need to be ruled out prior to diagnosis of granuloma annulare. Although the lesions are self-limiting, resolution can take up to several years and high potency topical steroids is usually recommended to hasten recovery for localized granuloma annulare. For those with more diffuse skin involvement, topical calcineurin inhibitors or immunomodulating medications are recommended. [6]
References:
1. Fox TC. Br J Dermatol 1895; 7:91.
2. Muhlemann MF, Williams DR. Br J Dermatol 1984; 111:325.
3. Li A, Hogan DJ, Sanusi ID, Smoller BR. Am J Dermatopathol 2003; 25:113.
4. Muhlbauer JE. J Am Acad Dermatol 1980; 3:217.
5. Güneş P, Göktay F, Mansur AT, et al. J Cutan Pathol 2009; 36:838.
6. Jain S, Stephens CJ. Br J Dermatol 2004; 150:1042.
Image Challenge: Week 28 - Friday, October 16, 2020

A 23-year-old South Asian-American male with no significant past medical history presents with a blue-black papule on the left lower leg. He recalls having the lesion for as long as he can remember without any inciting events or traumas. To his knowledge, it has not changed in size, shape, or color. He does not endorse any associated pain, bleeding, or drainage. He has no similar lesions and no family history of skin cancer. What is the most likely diagnosis?
A) Atypical Nevus
B) Common Blue Nevus
C) Dermatofibroma
D) Melanoma
E) Spitz Nevus
Correct Answer: B) Common Blue Nevus
Incorrect Answers:
A) Atypical nevi, (aka dysplastic nevi) are acquired or congenital lesions that typically present as nevi greater than 5mm, variegated in color with an erythematous background, and have an irregular and indistinct border. The diagnosis of dysplasia is made histologically, determined by the presence of disordered melanocytic proliferation in the epidermis, a fibrotic response in the dermis, and/or cytologic atypia. While the presence of atypical nevi does not necessarily increase an individual’s risk for skin cancer, those with an increasing number of atypical nevi and a family history of melanoma are at an increased risk. If the lesion was acquired in adulthood, has changed in size or morphology, or has had any associated symptoms of bleeding or itching, it can be removed by excisional or a deep shave excision for further evaluation. [1]
C) Dermatofibromas are tan to dark brown, hard dermal nodules or papules more commonly found in young adults. The diagnosis is made clinically as the lesion is firm when palpated and dimples when pinched (“dimple sign”). While a dermatofibroma does not require treatment, further work-up may be warranted to distinguish it from malignant lesions. Histologically, the epidermis is thickened and hyperpigmented while an aggregate of densely packed collagen with fibroblasts is present in the dermis. [1]
D) Melanoma is a cancerous neoplasm of pigment-forming cells, melanocytes, and nevus cells that typically presents an irregularly-shaped, colored papule or plaque. The ABCDE criteria (asymmetry, irregular border, color variegation, diameter greater than 6mm, and evolves or changes in size, shape, or color) is used to assess suspicious lesions. On observation, melanoma often differs significantly from other moles, appearing as an “ugly duckling.” A narrow excisional biopsy can confirm the diagnosis and specific subtype. With an early diagnosis, excisional removal is curative but melanomas that are greater than 1mm in thickness require further workup of the lymph nodes to evaluate for metastasis and treat accordingly. [1]
E) Spitz nevus is a smooth, round, scaling pink nodule that more commonly presents in children and fair-skinned individuals. While benign, the resemblance to melanoma does make clinical diagnosis a challenge. Under dermatoscopy, the Spitz nevus appears as a uniform, rounded structure with punctate or rounded vessels and if pigmented will show a globular pattern early on and will appear homogenous in color at later stages. [2] Histologically, the lesion is composed of spindle and epithelioid cells. [1]
Common Blue Nevus
Shara Chopra, BS, BA; Matthew F. Helm, MD; Alexandra Flamm, MD; Joslyn Sciacca Kirby, MD; Brian Green, DO
A 23-year-old South Asian-American male with no significant past medical history presents with a blue-black papule on the left lower leg. He recalls having the lesion for as long as he can remember without any inciting events or traumas. To his knowledge, it has not changed in size, shape, or color. He does not endorse any associated pain, bleeding, or drainage. He has no similar lesions and no family history of skin cancer. On physical exam, an 8 x 4 mm, blue-black symmetric, and sharply demarcated papule was observed on the left lower leg. The rest of his skin exam was unremarkable. Given the history of the lesion, lack of warning signs indicating malignancy, and observations under dermatoscopy, the lesion was diagnosed as a common blue nevus. The patient was advised to continue to watch the lesion for changes that could indicate malignancy. It has been 7 years since this diagnosis, and the nevus remains unchanged.
The common blue nevus is a benign neoplasm of dermal melanocytes presenting as a blue or blue-black papule or nodule that is well-demarcated and symmetric. More commonly found in young people and Asians, the common blue nevus is typically acquired, occurs in solitude, and often located on the face or extremities. [3] The blue color is a result of the Tyndall effect, or the reflection of dermal melanin because of its shorter wavelength. [4] The differential diagnosis for the common blue nevus includes the cellular blue nevus or malignant melanoma, both of which warrant further work-up. The cellular blue nevus, which is more likely to develop into a malignant blue nevus, differs in presentation as it is more common in middle-aged individuals, can be greater than a centimeter in size, and is often located on the buttock or sacrococcygeal region. If the lesion has changed in size or morphology or follows the ABCDE criteria used to assess malignant melanoma, excisional biopsy is warranted to make the distinction. Under dermatoscopy, it appears as a homogenous steel-blue color with a ground-glass pattern. Histologically, the common blue nevus appears as a wedge of proliferating spindle cells, dendritic melanocytes, and melanophages in a sclerotic dermis or subcutis. [3] Because the prognosis of a common blue nevus is good and does not require removal, the lesion should be observed for changes that would signify malignancy and would warrant a biopsy.
References:
1. Marks J G, Miller J J. Lookingbill and Marks Principles of Dermatology, 6e. Philadelphia: Elsevier. 2019.
2. Spitz Naevus. 2003. Retrieved from https://dermnetnz.org/topics/spitz-naevus/
3. Austad SS, Athalye L. Blue Nevus. In: StatPearls. Treasure Island (FL): StatPearls Publishing; August 8, 2020.
4. Blue Naevus. 2018. Retrieved from https://dermnetnz.org/topics/blue-naevus/
Image Challenge: Week 27 - Friday, October 9, 2020

A 21-year-old female with a history of polycystic ovarian syndrome (PCOS), recently started on spironolactone, presents to clinic with hand swelling and burning on and off for 1 month. She first noticed it when she was taking a shower and her hands were exposed to the warm water. Both palms initially began to sting and then developed swelling and blistering that completely resolved within 2 hours of drying. The condition continues to present every time she submerges her hands in water regardless of the temperature. The picture was taken after soaking her hands in water for 2 minutes. What is the most likely diagnosis?
A) Aquagenic acrokeratoderma
B) Aquagenic pruritis
C) Aquagenic urticaria
D) Contact dermatitis
E) Psoriasis
Correct Answer: A) Aquagenic acrokeratoderma
Incorrect Answers:
B) Aquagenic pruritis is characterized by prickling, burning and stinging of the skin within 30 minutes of contact with water. There are typically no associated skin findings. The condition usually begins in the legs before generalizing to the rest of the body with sparing of the head, palms, and soles. Aquagenic pruritis is rarely a primary disorder and instead more commonly secondary to a systemic disease such as polycythemia vera or another skin condition. Treatments are targeted at improving the underlying condition. There are also options for decreasing symptoms including alkalization of bath water, broadband UVB or PUVA, or capsaicin cream. [1]
C) In aquagenic urticaria, pruritic wheals develop over the body after contact with water. The condition often spontaneously resolves within an hour of onset. The pathogenesis is unknown, although it resembles a form of urticaria called cholinergic urticaria. [1]
D) Contact dermatitis is an inflammatory condition from chemical or physical agents causing an immune system reaction to the affected skin. [1] There are two types of contact dermatitis: irritant and allergic. [2] It is often associated with occupational exposures. Symptoms include stinging and burning at the site and may present with erythema, edema, and bullae. [1]
E) Psoriasis is characterized by well demarcated erythematous papules, patches, and plaques with silvery scale. Psoriasis plaques are typically found on the scalp, elbows and knees although they can be found anywhere on the body. [2]
Aquagenic Acrokeratoderma
Abigail Washington, BA; Matthew F. Helm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD; Alexandra Flamm, MD
A 21-year-old female with a history of polycystic ovarian syndrome (PCOS), recently started on spironolactone, presents to clinic with hand swelling and burning on and off for 1 month. She first noticed it when she was taking a shower and her hands were exposed to the warm water. Both palms initially began to sting and then developed swelling and blistering that completely resolved within 2 hours of drying. The condition continues to present every time she submerges her hands in water regardless of the temperature. In the clinic, the skin of both palms is completely normal with no signs of an underlying skin condition. After submerging her hands in room temperature water for 5 minutes, the characteristic translucent or whitish papules appear and then resolve within an hour of drying. The diagnosis of aquagenic acrokeratoderma is made clinically with the patient history, physical exam, and results from the water challenge. The patient is recommended to wear gloves or avoid contact with water and given topical barrier creams. Although the spironolactone was not discontinued, her condition spontaneously resolved after 1 year and she has been in remission for 5 years.
Aquagenic acrokeratoderma, also known as aquagenic wrinkling of the palms and soles, is more common in women and often presents during the second decade of life. [1] The condition may be genetic with either autosomal dominant or recessive inheritance or associated with the use of medications including cyclooxygenase-2 inhibitors and spironolactone. [3] The exact pathogenesis is unknown at this time, although aquagenic acrokeratoderma is often associated with cystic fibrosis suggesting that the development of lesions may be linked to sweat composition. Some other hypotheses include abnormal regulation of eccrine ducts as well as structural or functional defects in the stratum corneum. The diagnosis can be made with patient history and clinical findings. The condition can be triggered in a clinical setting with immersion of the patient’s hands in water as clinicians observe for the “hand-in-the-bucket sign” or development of the characteristic lesions. [3] The main treatment is avoidance of water. Other topical drying agents may be useful such as aluminum chloride hexahydrate or salicylic acid. [3]
References:
- Bolognia J, Schaffer J, Cerroni L. Dermatology. 4th ed. Philadelphia: Elsevier Saunders; 2018.
- Marks JG, Jr, Miller JJ(, Lookingbill DP, Marks JG, Jr. Lookingbill and Marks' Principles of Dermatology. Sixth ed. ELSEVIER; 2019.
- Wang, F., Zhao, Y.‐K., Luo, Z.‐Y., Gao, Q., Wu, W., Sarkar, R. and Luo, D.‐Q., Aquagenic cutaneous disorders. JDDG. 2017;15: 602-608. doi:1111/ddg.13234
Image Challenge: Week 26 - Friday, October 2, 2020

A 24-year-old male presents to clinic with multiple soft, mobile, painless masses on his left forearm, right lower abdomen, left upper abdomen, and right arm. The first mass appeared nine years ago (left forearm) measuring at the size of a half-dollar, and the three smaller masses have appeared over the years. None of the masses have grown in size. He does not recall any inciting events or trauma to these areas and does not recall having any family members with similar masses. He has not formally sought treatment. The patient does not endorse any longstanding history of fever, chills, or weight loss since the onset of the first mass. What is the most likely diagnosis?
A) Abscess
B) Epidermal Inclusion Cyst
C) Hibernoma
D) Lipoma
E) Liposarcoma
Correct Answer: D) Lipoma
Incorrect Answers:
A) Abscess: a collecting cavity of pus due to an acute bacterial infection. The most common pathogens include Staphylococcus aureus, Methicillin-resistant Staphylococcus aureus, and Streptococcus pyogenes. Abscesses present as an erythematous, fluctuant nodule that is warm, swollen, and painful. Lymphadenopathy and fever may also be present. Some risk factors include trauma, surgery, and intravenous drug use. Diagnosis is typically clinical, but a culture of the purulent material within the abscess can be confirmatory. Treatment options include incision and drainage and antibiotics. [1]
B) Epidermal Inclusion Cyst: a benign cyst filled with keratin and lipid debris deriving from the infundibulum or upper portion of the hair follicle. The cyst capsule is usually made of epithelium-like endothelial cells. Etiology is likely due to an obstructed pilosebaceous unit. Epidermal inclusion cysts are twice as likely to occur in men and are commonly seen in some genetic disorders, such as Gardner Syndrome and Basal Cell Nevus Syndrome. They present as a firm, mobile, flesh-colored papule or nodule with a central punctum that may extract foul-smelling yellow-white debris. Diagnosis is clinical, but an ultrasound and biopsy can be completed. Surgical excision with an intact capsule is most effective in reducing the rate of recurrence and histological examination of the cyst contents is recommended to ensure malignancy is not present. Smaller, asymptomatic cysts do not need to be removed. Complications include infection, cyst recurrence, and scarring. [2]
C) Hibernoma: a rare, benign brown fat tumor containing a capillary network. They commonly arise in the thigh, trunk, and chest wall as a painless, mobile, and slow-growing mass in adult males ages 30-40. [3] The etiology of hibernomas is not well understood, but chromosome 11q13-21 structural rearrangements have been seen. Biopsy of the mass typically shows a mixture of stromal cells as well as brown and white fat cells with multivacuolation, granular cytoplasm. Surgical excision of the tumor is curative. [4]
E) Liposarcoma: a fat tissue tumor and is the second most common soft tissue sarcoma after rhabdomyosarcoma. There are many different subtypes: well-differentiated, dedifferentiated, myxoid, round cell, and pleomorphic, all of which have varying severities. The etiology of liposarcomas is largely unknown and these tumors are largely asymptomatic, generally arising in the extremities. Changes in the size of the mass, its level of depth with or without pain, and non-specific constitutional symptoms may further support liposarcoma as an official diagnosis. Biopsy is performed to confirm the diagnosis of more superficial tumors and CT/MRI is used for deeper tumors. Treatment greatly depends on the location, size, and subtype of liposarcoma. Surgery is the mainstay treatment; however, chemotherapy and radiation therapy are considered for unresectable tumors. [5]
Lipoma
Brittainy Hereford, BS; Matthew F. Helm, MD; Alexandra Flamm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD
A 24-year-old male presents to clinic with multiple soft, mobile, painless masses on his left forearm, right lower abdomen, left upper abdomen, and right arm. The first mass appeared nine years ago (left forearm) measuring at the size of a half-dollar, and the three smaller masses have appeared over the years. None of the masses have grown in size. He does not recall any inciting events or trauma to these areas and does not recall having any family members with similar masses. He has not formally sought treatment. The patient does not endorse any longstanding history of fever, chills, or weight loss since the onset of the first mass. Upon physical exam, four soft masses were found – one on his left forearm (approximately 1.2 cm in diameter), one superficial to the left 9th rib (approximately 3 mm in diameter), one in the right lower quadrant of the abdomen (approximately 6 mm in diameter), and another near the right medial bicep (approximately 9 mm in diameter). The rest of his exam was non-contributory. His primary care physician gave him a clinical diagnosis of lipoma.
Lipomas are the most common benign mesenchymal tumors and tend to occur in adults. They present as a slow-growing, painless, soft mass commonly less than 5 cm in diameter and seen in the extremities, trunk, and neck. The etiology of lipomas may be due to 12q13-15 aberrations, 6p21-23 rearrangements, 13q deletions, HMGA2 (12q14.3) gene recombination. Histologic features of a lipoma include mature adipocytes with a thin, hypocellular septa and thin walled capillaries. Nuclear atypia is not present, and the presence of fat necrosis and inflammation may be indicative of post-traumatic changes. Lipomas are curative with complete resection; however intramuscular and intermuscular lipomas have the greatest risk of recurrence (up to 20%). It is very rare for a benign lipoma to transform to an atypical lipomatous tumor or liposarcoma. [4]
References:
1. Marks J G, Miller J J. Lookingbill and Marks Principles of Dermatology, 6e. Philadelphia: Elsevier. 2019.
2. Epidermoid Cyst. 2020. Retrieved from https://dermnetnz.org/topics/epidermoid-cyst/
3. Hibernoma. 2020. Retrieved from https://dermnetnz.org/topics/hibernoma/
4. Mentzel T, Brenn T. Lipogenic Neoplasms. In: Kang S, Amagai M, Bruckner AL, Enk AH, Margolis DJ, McMichael AJ, Orringer JS. Eds. Fitzpatrick's Dermatology, 9e. McGraw-Hill. 2019.
5. Livingston J, Conley A, Ravi V, Patel S. Soft tissue and bone sarcomas. Kantarjian HM, Wolff RA. Eds. The MD Anderson Manual of Medical Oncology, 3e. McGraw-Hill. 2016.

A 48-year-old patient with a past medical history GERD, spinal stenosis, hypertension, and bipolar I disorder presents with a diffuse rash that he states began 20 years ago while serving a prison sentence. He states the rash initially began bilaterally on his legs and has spread to involve both upper extremities and his torso. He admits to intense pruritis when exposed to heat like warm showers or sunlight. He denies fever, chills, nausea, vomiting, diarrhea, chest pain, episodes of syncope, changes in vision, numbness, changes in gait, increased bruising or mucocutaneous bleeding, and shortness of breath. He does try to avoid taking NSAIDs because they make him “itchy”. He also states that after scratching his skin he develops hives which resolve over time. He has 20-year pack history but quit 8 years ago and denies recreational drug use. On physical exam there are salmon-colored macules coalescing into bilaterally on both lower and upper extremities with sparing of the face, palms and soles, and mucosal membranes. What is the most likely diagnosis?
A) Acute HIV exanthem
B) Leukocytoclastic vasculitis
C) Prurigo pigmentosa
D) Secondary syphilis
E) Systemic mastocytosis
Correct Answer: E) Systemic mastocytosis
Incorrect Answers:
A) Acute HIV exanthem- presents as an eruption of non-pruritic diffuse erythematous maculopapular lesions. Lesions are typically distributed on the chest with central confluence but may vary. Lesions may be accompanied by fever, fatigue, headache, lymphadenopathy, pharyngitis, myalgias, and diarrhea. Acute symptoms typically occur one to four weeks after transmission and persists for two to four weeks. These symptoms tend to correspond to a drop in CD4 count and rise in viral load. Men who have sex with men, intravenous drug abuse, and high-risk heterosexual intercourse are all risk factors for HIV, however, fever of unknown origin should warrant workup given non-specific symptoms. Acute HIV infection precedes the generation of antibodies needed to perform an ELISA. Therefore, suspected cases should undergo workup with p24 antigen or HIV viral RNA. Initiation of treatment with highly active antiretroviral therapy during active infection remains controversial, although progression to HAART is ultimately recommended. [1]
B) Leukocytoclastic vasculitis- is a small-vessel cutaneous vasculitis characterized by neutrophilic inflammation. Lesions typically present as symmetric palpable purpura but may also appear as port-wine papules, urticarial, ulcerative, vesicular, pustular, and nodular. They are typically are distributed on the lower extremities and appear in crops with associated pruritis, pain, or burning. Although 45-55% of cases are idiopathic a sizable amount of cases are due to infections, connective tissue disease, drug reactions, or lymphoproliferative disorders or malignancies. As such, workup of leukocytoclastic vasculitis includes skin biopsy with H&E and direct immunofluorescence and various labs to elucidate underlying pathology as well as evaluation for potential extracutaneous manifestation of vasculitis. Treatment varies but typically begins with symptomatic care and prednisone tapers followed by steroid sparing agents in chronic or refractory cases. [2]
C) Prurigo pigmentosa- presents as recurrent eruptions of pruritic, erythematous macules and papules which tend to coalesce and are characterized by reticulated pigmentation. They are symmetrically distributed on the trunk with a predilection for the upper back, sacrum, abdomen, and chest and predominantly occur in patients of East Asian descent. Some studies have demonstrated evidence of correlation with ketogenic diet, however, pathology seems to suggest a reactive process. Diagnosis is difficult and is based on characteristic histopathology and failure of the lesion to respond to topical steroids. Therapy consists of oral minocycline with a fairly robust response. [3]
D) Secondary syphilis- presents as non-pruritic red-brown or copper macules or papules which characteristically involve the palms and soles. Oral and genital mucosa have been known to be involved. Syphilis is a sexually transmitted disease due to treponema pallidum spirochetes. The disease may be asymptomatic or progress from a primary infection with a non-tender chancre to diffuse maculopapular rash and ultimately lead to neural involvement resulting in loss of proprioception and ocular reflexes. Diagnosis is based on syphilis serology (treponemal test, RPR or VDRL). In some instance biopsy of affected skin may be useful. Treatment involves intramuscular penicillin. Workup for concurrent sexually transmitted diseases should also be performed. [4]
Systemic Mastocytosis
Robert Fort, BA; Alexandra Flamm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD; Matthew F. Helm, MD
A 48-year-old patient with a past medical history GERD, spinal stenosis, hypertension, and bipolar I disorder presents with a diffuse rash that he states began 20 years ago while serving a prison sentence. He states the rash initially began bilaterally on his legs and has spread to involve both upper extremities and his torso. He admits to intense pruritis when exposed to heat like warm showers or sunlight. He denies fever, chills, nausea, vomiting, diarrhea, chest pain, episodes of syncope, changes in vision, numbness, changes in gait, increased bruising or mucocutaneous bleeding, and shortness of breath. He does try to avoid taking NSAIDs because they make him “itchy”. He also states that after scratching his skin he develops hives which resolve over time. He has 20-year pack history but quit 8 years ago and denies recreational drug use. On physical exam there are salmon-colored macules coalescing into patches bilaterally on both lower and upper extremities with sparing of the face, palms and soles, and mucosal membranes. Gentle stroking of the skin created localized wheals. A punch biopsy of the skin was performed with Giesma stain which revealed mastocytes. Liver function tests, CBC with differential, urinalysis, and IgE levels were normal. Tryptase levels were elevated at 53.6. Due to concern for systemic mastocytosis the patient was referred to hematology-oncology. Bone marrow biopsy was performed revealing systemic mastocytosis without KIT mutation. He was therefore given cetirizine 10mg, ranitidine 150mg BID, and triamcinolone 0.1% topical cream for symptomatic control of pruritis. He will follow annually with dermatology and hematology-oncology.
Mastocytosis is due to the accumulation of an excessive amount of mast cells within the skin with or without visceral involvement. Because mast cells contain vasoactive mediators required for innate immune defense, degranulation can result in symptoms seen in allergic and anaphylactic reactions. The severity of this response is variable and is often more severe if organs and bone marrow are involved. Organ involvement appears to vary by age with cutaneous mastocytosis occurring predominantly in children and systemic in adults. The most common cutaneous manifestation is urticaria pigmentosa or maculopapular cutaneous mastocytosis which is characterized by small yellow/tan to red/brown macules or papules. These lesions tend to coalesce and characteristically involved the upper and lower extremities as well as the torso. Palms and soles, face, and scalp are generally spared in adults but may be involved in children. Darier’s sign is a characteristic physical finding which is the development of localized urticaria and erythema within minutes of physical irritation of the skin (i.e scratching or rubbing). Systemic mastocytosis may involve the gastrointestinal tract, bone marrow, or other organs and is typically preceded by cutaneous manifestations. Mast cell mediators may lead to flushing, hypotension, syncope, recalcitrant peptic ulcers, diarrhea, osteoporosis, neuropsychiatric disturbances, and in severe cases anaphylaxis and sudden cardiovascular collapse. These symptoms tend to occur in response to physical or pharmacologic stimuli that lead to massive mast cell degranulation. Diagnosis begins with a punch biopsy of the skin with staining for mast cells. All adults should undergo systemic workup with complete blood count with differential, liver function tests, tryptase levels, and a bone marrow biopsy. KIT mutational analysis should be performed on bone marrow or peripheral blood to evaluate for monoclonal or idiopathic mast cell expansion in order to tailor therapy. Once the diagnosis is established patients should be maintained with H1 and H2 blockers and mast cell stabilizers to reduce the severity of symptoms. Topical corticosteroids and PUVA therapy may be used to reduce the appearance of cutaneous hyperpigmentation, and in cases of KIT mutations tyrosine-kinase inhibitors like Imatinib may be used. Mast cell degranulators such as NSAIDs, narcotics, anticholinergics, aspirin, and alcohol should be avoided to prevent episodes of mast cell activation. [5]
References:
1. Alto , W. A., & Clarcq, L. (1999). Cutaneous and systemic manifestations of mastocytosis.
American Family Physician, 3047-3054.
2. Chu , C., & Selwyn , P. A. (2010). Diagnosis and initial management of acute HIV infection.
American Family Physician, 1239-144.
3. Ely , J. W., & Seabury Stone , M. (2010). The Generalized Rash: Part I. Differential Diagnosis.
American Family Physician, 726-734.
4. Goeser , M. R., Laniosz, V., & Wetter , D. A. (2014). A practical approach to the diagnosis,
evaluation, and management of cutaneous small-vessel vasculitis . American Journal of
Clinical Dermatology , 299-306.
5. Whang , T., Kirkorian , Y. A., Krishtul , A., Phelps , R., & Shim-Chang, H. (2011). Prurigo
pigmentosa: Report of two cases in the United States and review of the literature . Dermatology Online , Dermatology Online Journal, 17(12). Retrieved from https://escholarship.org/uc/item/6rv324m4.
Image Challenge: Week 25 - Friday, September 25, 2020

A 20-year-old male currently attending college presents to the clinic for a routine check-up with a painless, shiny red, raised lesion on the middle of his chest. He first noticed the lesion three years ago, and states that the lesion has gradually grown in size over the past few years despite various attempts to treat the lesion with topical creams. He is otherwise healthy with no significant past medical history. What is the most likely diagnosis?
A) Acne vulgaris
B) Atrophic scar
C) Hypertrophic scar
D) Keloid scar
E) Wart
Correct Answer: D) Keloid scar
Incorrect Answers:
A) Acne vulgaris is a common skin condition that affects nearly 80% of the adolescent population. It is a result of a multitude of factors, including colonization by Cutibacterium acnes leading to inflammation, increased sebum production, and follicular hyperkeratosis. Genetics, hormones, and other external factors are also implicated in the pathogenesis of acne. Thus, they are commonly seen in adolescents during puberty. Treatment of acne varies based on severity, but common options include topical benzoyl peroxide, antibiotics, and retinoid therapy. A common sequelae of acne vulgaris is scarring and may affect up to 95% of patients with acne, with the most common type of scar being an atrophic scar. [1]
B) Atrophic scars are a type of skin lesion that appear flat and depressed below the skin, likely due to enzymatic degradation of collagen. They are typically seen on the face and are the most common type of scar to appear in patients with acne vulgaris but can also appear following chickenpox. Atrophic scars can be further classified based on their appearance into three main types: ice pick, rolling, and boxcar. A number of treatment options exist for atrophic acne scars, including but not limited to chemical peels, punch techniques, laser treatment, and dermabrasion. [1]
C) Hypertrophic scars are a type of skin lesion that results from high fibroblast proliferation and excessive collagen deposition during the wound healing process. Hypertrophic scars appear as raised scar tissue that may be firm and erythematous and may be also be accompanied by pruritus. They present similarly to keloid scars (see below), but the severity of the collagen deposition is not quite to the degree of a keloid scar. Compared to keloid scars, hypertrophic scars are typically confined to its original boundaries, regress spontaneously, and respond well to treatment. Treatment options include resection, cryotherapy, and steroid injections. [2]
E) Warts are skin lesions resulting from hyperkeratosis of the epidermis and are commonly caused by human papillomavirus. There are various types of warts, including common warts, flat warts, and plantar warts, and can present all over the body, including the elbows, knees, hands, feet, and face. Warts typically present as flesh-colored papules or plaques. Treatment typically involves a course of topical salicylic acid but can also involve cryotherapy or surgical excision. [3]
Keloid Scar
Jay Yang, BS; Matthew F. Helm, MD; Alexandra Flamm, MD; Joslyn Sciacca Kirby, MD; Brian Green, DO
A 20-year-old male currently attending college presents to the clinic for a routine check-up with a painless, red, raised lesion on the middle of his chest. He first noticed the lesion three years ago, and states that the lesion has gradually grown in size over the past few years. He is otherwise healthy with no significant past medical history. On physical exam, additional similar lesions of varying size were appreciated on the upper back and shoulders. The rest of the exam was unremarkable. Based on the history and exam, the patient was diagnosed with a keloid scar. Given the benign nature of the lesion and the minimal impact on the patient’s life, no treatment was pursued.
Keloid scars are skin lesions that result from high fibroblast proliferation and excessive collagen deposition during the wound healing process. They are similar to hypertrophic scars, but notably differ in a few ways: hypertrophic scars are typically confined to the boundaries of the original wound, regress with time, and are more responsive to treatment, while keloid scars grow beyond the boundaries of the original lesion, do not regress spontaneously, and are more resistant to treatment. Keloid scars are commonly seen in patients with darker skin, with an incidence of 4.5-16% in Black and Hispanic populations. They are seen equally in men and women, and while they can affect people of any age, they most commonly affect patients between the ages of 10-30 years old. Keloid scars vary in size from a few millimeters to a few centimeters or more in diameter. Common areas for keloid scars include the ears, cheeks, shoulders, chest, upper arms, and upper back. Other potential clinical findings include pain, pruritus, and burning. Treatment options for keloid scars vary, but first-line therapy typically involves intralesional Kenalog injections. Surgical excision, radiotherapy, cryotherapy, and compression therapy are a few other commonly used treatment methods. Unfortunately, most keloid scars recur even following treatment. Treatment options are often combined in order to reduce the chance of recurrence. However, prevention of keloid scars remains the best treatment option. [2]
References:
1. Gozali MV, Zhou B. Effective treatments of atrophic acne scars. J Clin Aesthet Dermatol. 2015;8(5):33-40.
2. Alster TS, Tanzi EL. Hypertrophic Scars and Keloids. American Journal of Clinical Dermatology. 2003;4(4):235-243.
3. Shenefelt PD. Nongenital Warts. https://emedicine.medscape.com/article/1133317-overview. Published March 22, 2020. Accessed September 16, 2020.
Image Challenge: Week 24 - Friday, September 18, 2020

A 54-year-old female with a past medical history of seborrheic keratosis presents to clinic with multiple small papules on her trunk and arms that have been increasing in size and number very slowly over the years. The patient did not attempt to seek treatment until now. The red papules are not itchy or painful. Upon physical exam, multiple 1-3mm bright red papules were diffusely located on trunk and arms. The rest of her exam was non-contributory. What is the most likely diagnosis?
A) Amelanotic melanoma
B) Cherry angioma
C) Keratosis pilaris
D) Petechiae
E) Spider nevus
Correct Answer: B) Cherry Angioma
Incorrect Answers:
A) Amelanotic melanomas are classically skin colored papules or nodules that sometimes can have color variations of pink or red. The early lesion is often nearly symmetric and displays well defined borders that can be difficult to diagnose using the classic ABCDE criteria. Delay in diagnosis often occurs as a result until it reaches an advanced stage and can therefore have poor prognosis given its significant risk for metastasis. The risk factors of melanoma in general include ultraviolet radiation exposure, lower Fitzpatrick skin type, older age, family history and immunosuppression. An immediate full-thickness excision biopsy is the gold standard diagnostic test in all suspicious lesions. Treatment is based on staging but will usually require a larger wide local excision, and possible sentinel lymph node biopsy. Additional therapies for unresectable or metastatic tumors include targeted systemic therapies such as BRAF and PD-1 inhibitors. [1]
C) Keratosis pilaris is a disorder of keratinization of hair follicles of the skin. It is an extremely common benign condition that manifests as small, rough folliculocentric keratotic papules that can develop mild erythema around the hair follicles, particularly the outer-upper arms and thighs. It affects 50-80% of adolescents and around 40% of adults, improving with aging. Medications, such as nilotinib, have been implicated as causes. Familial cases often have a genetic component. The etiology of keratosis pilaris is not fully known although it’s often associated with dry skin and a process of faulty keratinization. Diagnosis of keratosis pilaris is based on a typical skin appearance on upper arms. Treatment in mild forms includes over-the-counter emollients. Other treatments can include: alpha hydroxy acid lotions, salicylic acid, retinoic acid products, and chlorine dioxide complex. [2]
D) Petechiae are small pin-point like red macules caused by hemorrhage of capillaries within the dermis. They have a wide variety of etiologies including prolonged straining, coagulopathy (Vitamin C/K deficiency) and can be primary or secondary to infections, autoimmune disease or medications. The petechiae do not need to be treated; however, work-up and treatment for an underlying condition is indicated when suspected. [3]
E) Spider nevus, a common benign vascular lesion, ranges in size from 1-10mm in diameter, with a central red arteriole (punctum) surrounded by radial pattern of thin-walled capillaries. In the general population, it is present in 10-15% of adults and children with no underlying medical conditions. Sporadic spider nevus is associated with female sex and aging. Other conditions associated with spider nevus include: thyrotoxicosis, estrogen-excess states (e.g., pregnancy or oral contraceptive usage), and liver diseases (particularly in alcoholic liver cirrhosis). Patients with extensive spider nevi should be evaluated for underlying associated medical conditions. If change is noted of a solitary lesion, biopsy should be considered to rule out other etiologies. The lesions often resolve spontaneously, especially in children, or following the resolution or treatment of associated medical conditions. Electrodesiccation and vascular laser treatment both can be effective for bothersome primary spider nevi, although recurrences are common. [4]
Cherry Angioma
Sage Gee, BS; Matthew F. Helm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD; Alexandra Flamm, MD
A 54-year-old female with a past medical history of seborrheic keratosis presents to clinic with multiple small papules on her trunk and arms that have been increasing in size and number very slowly over the years. The patient did not attempt to seek treatment until now. The red papules are not itchy or painful. Upon physical exam, multiple 1-3mm bright red papules were diffusely located on trunk and arms. The rest of her exam was non-contributory. What is the most likely diagnosis?
Cherry Angiomas are the most common cutaneous vascular proliferations; they appear as small red macules or papules. They are benign lesions formed by proliferation of dilated venules and limited to the skin. Cherry angiomas are very common in all age and races; however, the number and size of the lesions do increase past patient’s 3rd or 4th decade of life. The cause of cherry angioma is not clear, and genetic analysis has shown that they often carry specific somatic missense mutations in GNAQ and GNA11 genes, which are involved in other vascular and melanocytic proliferations. Cherry angiomas can also be observed in patients with malignancies such as multicentric Castleman disease (MCD) and other lymphoproliferative diseases. Though the diagnosis of cherry angioma is usually made clinically, a shave or punch skin biopsy can be used in rare circumstances when malignancy is suspected. Medical intervention is generally not indicated unless cosmetically bothersome or in situations of irritation or hemorrhage. Locally destructive treatments, such as vascular laser and electrodessication, can be effective in these situations. [4]
References:
1. McClain, S. E., Mayo, K. B., Shada, A. L., Smolkin, M. E., Patterson, J. W., & Slingluff, C. L. Amelanotic melanomas presenting as red skin lesions: a diagnostic challenge with potentially lethal consequences. Int J Dermatol. 2012 Apr; 51(4): 420–426
2. Hwang S, Schwartz RA. Keratosis pilaris: a common follicular hyperkeratosis. Cutis. 2008 Sep. 82(3):177-80
3. Oskay T, Kutluay L, Kaptanoglu A et al. Autoimmune progesterone dermatitis. Eur J Dermatol 2002; 12: 589–91
4. Dawn G, Gupta G. Comparison of potassium titanyl phosphate vascular laser and hyfrecator in the treatment of vascular spiders and cherry angiomas. Clin Exp Dermatol. 2003 Nov. 28(6):581-3
Image Challenge: Week 23 - Friday, September 11, 2020

A 61-year-old female with a past medical history of polymyositis presents to the hospital with 6 weeks of decreased oral intake and episodes of delirium. The patient admits to a 50lb unintentional weight loss with a precipitous decline in activities of daily living over the past 3 months as well as significant fatigue. On examination of the oropharynx, the maxillary dentition is absent and there is a non-tender shaggy, brown, adherent plaque with sharp borders across the dorsal tongue. The patient denies fever, chills, night sweats, diarrhea, shortness of breath, oral ulcers, dysphagia, or odynophagia. She admits to occasional post-prandial nausea and vomiting and has a 10 pack-year smoking history but stopped smoking 30 years ago. What is the most likely diagnosis?
A) Black hairy tongue
B) Candidiasis
C) Lichen planus
D) Oral hairy leukoplakia
E) Oral mucosal squamous cell carcinoma
Correct Answer: A) Black hairy tongue
Incorrect Answers:
B) Candidiasis- presents as confluent, non-adherent, white plaques on the tongue, buccal mucosae, palate, or pharynx. Plaques are classically easy to remove and reveal an underlying erythematous surface. Due to overgrowth of Candida albicans, risk factors for thrush include dentures, inhaled corticosteroids, xerostomia, malnutrition, and immunocompromised states. Diagnosis is typically clinical but may be supplemented by smears, cultures, and stains that demonstrate pseudohyphae and budding yeast. Treatment is based on severity and ranges from topical or suspension preparations to systemic antifungals. [1]
C) Lichen planus- commonly presents as a painful, lacy-white, reticular lesion and hyperkeratotic plaques or papules located on the buccal mucosae, gingivae, or ventral tongue. There are multiple less common subtypes but the pathophysiology is a T-cell mediated immune reaction to basal keratinocytes. Etiology may be idiopathic, a lichenoid-drug reaction, or related to dental/oral allergens. Oral lichen planus is a chronic disease with 1.1% of patients developing oral squamous cell carcinoma. Diagnosis is clinical with histologic confirmation demonstrating band-like lymphocytic infiltration. Topical steroids are used to treat symptomatic lesions. Intralesional or systemic steroids as well as topical or systemic calcineurin inhibitors may be utilized in more severe or recalcitrant cases. [2]
D) Oral hairy leukoplakia- presents with non-tender, white, adherent, corrugate plaques on the lateral aspect of the tongue. Lesions may be unilateral or bilateral and presents predominantly in patients with an immunocompromised status. Thought the etiology is multifactorial it is clear that it is an EBV-related disease that occurs in the setting of significant immunosuppression. Diagnosis is clinical, however; its presence in the absence of known immunosuppression should prompt workup for HIV infection. Oral hairy leukoplakia carries no malignant potential and treatment is not required. However, underling HIV infection or immunosuppression should be addressed if present. Topical preparations of retinoids and podophyllin have been used as well as systemic antivirals, however, lesions tend to recur after discontinuation. [3]
E) Oral mucosal squamous cell carcinoma- presents in the setting of premalignant lesions like leukoplakia, erythroplakia, and leukoerythroplakia, or as an exophytic nodular mass with varying degrees of erythema. Lesions may occur anywhere but the tongue accounts for 50% of cases. Risk factors include tobacco use, alcohol use, radiation, premalignant oral lesions, human papillomavirus, and other sexually transmitted infections. Classification and prognosis are based on tumor, node, and metastasis staging with histologic grade correlation to tumor behavior. Histology is characterized by invasive islands of squamous epithelial cells that invade the basement membrane and surrounding structures. Treatment consists of a combination of wide surgical excision, neck dissection, radiation therapy, and chemotherapy. Prognosis is poor with a 5-year survival rate of 50% to 59%. [2]
Black Hairy Tongue
Robert Fort, BA; Alexandra Flamm, MD; Brian Green, DO; Matthew F. Helm, MD; Joslyn Sciacca Kirby, MD
A 61-year-old female with a past medical history of polymyositis presents to the hospital with 6 weeks of decreased oral intake and episodes of delirium. The patient admits to a 50lb unintentional weight loss with a precipitous decline in activities of daily living over the past 3 months as well as significant fatigue. On examination of the oropharynx, the maxillary dentition is absent and there is a non-tender shaggy, brown, adherent plaque with sharp borders across the dorsal tongue. The patient denies fever, chills, night sweats, diarrhea, shortness of breath, oral ulcers, dysphagia, or odynophagia. She admits to occasional post-prandial nausea and vomiting and has a 10 pack-year smoking history but stopped smoking 30 years ago. Dermatology was consulted and black hairy tongue was diagnosed based on a clinical history of prolonged decreased oral intake. She was given chlorhexidine mouth wash and a tongue scraper to aid in desquamation. She was instructed on daily oral hygiene. The main concern and likely the etiology of her tongue lesion was malnutrition in the setting of hypoactive delirium. Extensive workup did not reveal any organic cause. Neurocognitive workup resulted in a MOCA score of 17 with the most likely etiology being psychiatric versus neurologic in the setting of the recent loss of a family member. The patient was deemed to have capacity and she ultimately elected to go home to the care of her family. Further neurocognitive workup and psychiatric follow-up was scheduled.
Black hairy tongue is a benign condition resulting in hypertrophy of filiform papillae on the dorsal aspect of the tongue. This hypertrophy results in a carpet-like, adherent plaque with sharp borders that spares the tip, edges, and most posterior section of the tongue. Though it often appears black, the name is a bit of a misnomer as black hairy tongue actually ranges in color from brown/ yellow to green/blue. This variation in hue thought to be due to accumulation of fungi, bacteria, and other porphyrin producing chromogenic. Known risk factors are male sex, older age, smoking, alcohol use, and poor oral hygiene. Xerostomia-inducing agents like olanzapine or chlorpromazine and antibiotics like tetracyclines are known culprits as well. Ultimately, the pathophysiology is thought to stem from defective desquamation of the dorsal surface of the tongue which leads to elongated papillae. This is normally accomplished with normal mastication but can compromised in the absence of a well-rounded diet or in the presence of neurological or psychiatric illness. Black hairy tongue is self-limited with an excellent prognosis. Though primarily a cosmetic concern, patients may experience irritation, nausea, gagging, dysgeusia, metallic taste, and perceived halitosis. Diagnosis is based on intraoral exam and rarely requires the assistance of tongue biopsy. Black hairy tongue is a self-limited disease with an excellent prognosis. Management typically focuses on promotion of desquamation through the use of a soft toothbrush or tongue scraper in tandem with daily oral hygiene and a well-rounded high-fiber diet. Modifiable risk factors should be discontinued like smoking or alcohol consumption. Offending pharmaceutical agents may be changed if need be. In rare instances dental evaluation and electrodessication with a carbon dioxide laser may be required. [4]
References
1. Millsop, J. W., & Fazel, N. (2016). Oral candidiasis. Clinics in Dermatology, 487-494.
2. Maymone, M., Greer, R. O., Kesecker, J., Cherukuri Sahitya, P., Burdine, L. K., Cheng, A.-D., Vashi, N. A. (2019). Premalignant and malignant oral mucosal lesions: Clinical and pathological findings. Journal of the American Academy of Dermatology, 59-71.
3. Mangold, A. R., Torgerson, R. R., & Rogers, R. S. (2016). Diseases of the tongue. Clinics in Dermatology, 458-469.
4. Gurvits, G. E., & Tan, A. (2014). Black hairy tongue syndrome. World Journal of Gastroenterology, 10845-10850.
Image Challenge: Week 22 - Friday, September 4, 2020

An active 3-year-old girl with a past medical history of atopic dermatitis well controlled with triamcinolone 0.1% ointment presents to clinic with a pink, slightly scaling rash on the soles of her feet. The child reports pruritis but no other symptoms. Her father first noticed the rash 2 months ago and attempted treatment with over the counter Lamisil (topical terbinafine). The anti-fungal did not resolve the rash. No other treatments were tried. What is the most likely diagnosis?
A) Atopic dermatitis
B) Dyshidrotic eczema
C) Hand-foot-mouth disease
D) Juvenile plantar dermatosis
E) Tinea pedis
Correct Answer: D) Juvenile plantar dermatosis
Incorrect Answers:
A) Atopic dermatitis is a chronic, relapsing inflammatory skin condition that typically occurs in conjunction with other atopic conditions like asthma and allergies. Around 90% of children with atopic dermatitis will present by the age of 5 with 70-90% of childhood cases resolving by adulthood. Atopic dermatitis presents differently depending on the age of the patient and history of the disease. In childhood, atopic dermatitis presents as pruritic, lichenified plaques commonly on the flexor surfaces, such as the antecubital and popliteal fossa. Although, the patient in the case has a history of atopic dermatitis, it would be uncommon for it to present on the soles of the feet. The lesions in the case are not lichenoid in nature, making an atopic dermatitis exacerbation unlikely. [1]
B) Dyshidrotic eczema is a type of idiopathic eczema that occurs on the palms of the hands, soles of the feet, and sides of the fingers. It typically presents with pruritic vesicles filled with clear fluid. The vesicles can rupture and leave the skin desquamated. This type of eczema tends to be symmetrical and bilateral. Erythema is not a common morphologic feature of this type of eczema. In the case reported above, the presence of erythema and lack of vesicles on the soles is evidence that does not support the diagnosis of dyshidrotic eczema. [2]
C) Hand-foot-mouth disease (HFMD) is an illness commonly caused by the coxsackie A virus. HFMD is more prevalent in children but can occur in adults. The typical presentation consists of a child with symptoms of an upper respiratory infection (i.e. fever and sore throat) that develops ulcerative lesions in the mouth and papules/vesicles on the palms of the hands and soles of the feet. Erythema can surround the lesions on the hands and feet. The infection has a mild course that resolves on its own in about a week. The presented case has no vesicles or papules present and has had this rash for 2 months. [2]
E) Tinea pedis, colloquially known as athlete’s foot is a fungal infection of the feet. Common fungi that cause infection are Epidermophyton, Microsporum, and Trichophyton. There are multiple subtypes of tinea pedis including diffuse plantar, interdigital, and vesiculopustular. Of these, interdigital is the most common subtype in the non-elderly population. Interdigital tinea pedis presents with significant pruritis, scale, and can also cause erythema in between the digits of the feet, toe pads, and forefoot. Localized infections of tinea pedis can be treated with topical antifungals. In the case presented, topical antifungals were trialed with no resolution. [2]
Juvenile Plantar Dermatosis (JPD)
Ramon Govea, BS; Alexandra Flamm, MD; Brian Green, DO; Matthew F. Helm, MD; Joslyn Sciacca Kirby, MD
An active 3-year-old girl with a past medical history of atopic dermatitis controlled with triamcinolone 0.1% ointment presents to clinic with a pink, slightly scaling rash on the soles of her feet. The child reports pruritis, but no other symptoms. Her father first noticed the rash 2 months ago and attempted treatment with over the counter Lamisil (topical terbinafine). The anti-fungal did not resolve the rash. No other treatments were tried. On physical exam, there were multiple well demarcated, pink patches on the soles of the feet with slight scale and complete sparing of the arches. Mild desquamation of the pads of the toes was also present. The clinical diagnosis of juvenile plantar dermatosis was made. Treatment consisted of topical 0.1% triamcinolone ointment to the affected areas BID for the next 7-10 days.
Juvenile plantar dermatosis (JPD) is an eczematous dermatitis that commonly manifests in children from the age of 3 until puberty. It presents as patchy erythema predominantly on the forefoot and pads of the toes, where more pedal pressure and friction occurs. Desquamation and scale can occur with sparing of the toe webs and arches. JPD is more common in children with a personal or family history of atopy. JPD occurs when moist or wet feet are in constant friction with any material. The classic history is an active child in athletic, occlusive shoes where the socks get sweaty and are not changed frequently. Diagnosis is made based on history and clinical presentation. There are multiple approaches to treatment of JPD that begin with lifestyle modifications such as using shoes that allow for proper ventilation, drying the feet after very active sessions, changing socks frequently, and not wearing the same shoes all day. Topical steroids can be used in conjunction with lifestyle modifications. Most cases of JPD clear within 4 years of diagnosis. In the cases where suspected JPD does not clear with treatment, other diagnoses should be suspected like allergic contact dermatitis. [2]
References:
1. Eichenfield LF, Tom WL, Chamlin SL, et al. Guidelines of care for the management of atopic dermatitis: section 1. Diagnosis and assessment of atopic dermatitis. J Am Acad Dermatol. 2014;70(2):338-351. doi:10.1016/j.jaad.2013.10.010
2. James, W. D., Elston, D. M., Neuhaus, I. M., & Berger, T. G. Andrews' Diseases of the Skin: Clinical Dermatology. 12th Edition. Philadelphia, PA: Elsevier; 2016.
Image Challenge: Week 21 - Friday, August 28, 2020

A 79-year-old obese woman with a past medical history of diabetes, atrial fibrillation on apixaban, venous insufficiency, coronary artery disease status post stent placement, and hypertension treated with amlodipine presents to the hospital after a fall where she struck her head while at a nursing home. She is oriented to person but not place or time. On exam, both lower extremities display edema to the level of the mid-shin with concomitant circumferential, sharply marginated hyperpigmentation with erosions, crust, and wide-spread induration. A 1+ dorsalis pedis pulse can be appreciated bilaterally. The patient is not able to report how long her legs have looked like this but her husband states that they have progressed to this point over the past few years. What is the most likely diagnosis?
A) Cellulitis
B) Contact dermatitis
C) Deep venous thrombosis
D) Pretibial myxedema
E) Stasis dermatitis with lipodermatosclerosis
Correct Answer: E) Stasis dermatitis with lipodermatosclerosis
Incorrect Answers:
A) Cellulitis presents with an acute to subacute progression of a poorly defined erythematous patch that is accompanied by warmth, edema, and pain. Vesicles, bullae, pustules, and underlying necrosis or osteomyelitis may occur as well and can be associated with specific pathogens. Predisposing factors include trauma, IV drug abuse, diabetes, chronic venous insufficiency, lymphedema, and chronic inflammation. Cellulitis of the lower extremity is typically unilateral and accompanied by fever and leukocytosis. The most common pathogens include Staphylococcus aureus and Group A streptococcus. The presence of purulence should increase suspicion for methicillin resistant staphylococcus aureus. Cultures of bullae, pustules, and ulceration should be obtained when possible. Suspicion for osteomyelitis should prompt X-ray and MRI. Empiric antibiotic treatment should begin after cultures are drawn and continued until resolution.
B) Contact dermatitis can occur anywhere on the body but typically presents with erythematous patches or plaques. Acute presentations may also present with vesicles and bullae while chronic cases can present with fissures, cracking, and lichenification of the skin from chronic itching and trauma. Contact dermatitis is subclassified into allergic and irritant pathology. Both may occur simultaneously and are more likely to occur in conditions like stasis dermatitis. Irritant contact dermatitis is due to exposure to chemicals, soaps, plants and body fluids and typically presents with pruritic or painful erythematous patches or plaques with moderately well-defined borders. In comparison, allergic contact dermatitis is due to a Type IV delayed hypersensitivity to a topical antigen. Common causes include urushiol allergy, nickel, cosmetics, and rubber or plastic based compounds. Acute presentations vary but can range from erythematous patches and plaques with well-defined or geometric/polygonal borders to linear erythematous papules with weeping vesicles. Chronic presentations are characterized by erythematous, scaling lichenified plaques that extend beyond the point of initial contact. In both cases diagnosis is typically clinical. Patch testing may be used to identify allergic etiologies, however; avoidance of a suspected trigger is often diagnostic and therapeutic. [1]
C) Deep Venous Thrombosis (DVT) may present with unilateral lower-extremity edema, warmth, and erythema. Tenderness, pitting edema, and increased leg circumference >3cm in comparison to the other leg are sensitive findings that would support the diagnosis of DVT. Onset of pain may be sudden or progressive and can be accompanied by an inflammatory response leading to fever and leukocytosis. Risk factors include active malignancy, prolonged immobilization, recent surgery, family history, tobacco, and oral contraceptive use. Because DVT may progress to pulmonary embolism, diagnosis must be made with a combination of D-dimer and/or compression ultrasonography depending on pretest probability. DVT should be treated with anticoagulation therapy to prevent further clotting. Given the bilateral and chronic presentation in this current patient as well as her prophylactic use of apixaban, a DVT is highly unlikely.
D) Pretibial myxedema is an autoimmune manifestation of Grave’s disease and occasionally Hashimoto’s thyroiditis. It presents progressively, beginning in the pretibial region with raised waxy lesions that range from flesh-colored to a yellowish-brown hue with hyperhidrosis and a peau d’orange appearance. Diagnosis is typically clinical and supported by associated features like exophthalmos and other signs of hyperthyroidism as well as the fact that lesions are typically symmetrical with non-pitting edema unlike that which is seen in instances of chronic venous insufficiency. Histopathology is rarely required but will show mucin accumulation in the reticular dermis and subcutaneous tissue. Most cases are mild and treated with expectantly the underlying hyperthyroidism treatment. More severe cases may be treated with high-potency steroids under occlusive dressing or systemic-immunomodulation. [2]
Stasis Dermatitis with Lipodermatosclerosis
Robert Fort, BA; Alexandra Flamm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD
A 79-year-old obese woman with a past medical history of diabetes, atrial fibrillation on apixaban, venous insufficiency, coronary artery disease status post stent placement, and hypertension treated with amlodipine presents to the hospital after a fall where she struck her head while at a nursing home. She is oriented to person but not place or time. On exam, both lower extremities display edema to the level of the mid-shin with concomitant circumferential, sharply marginated hyperpigmentation with erosions, crust, and wide-spread induration. A 1+ dorsalis pedis pulse can be appreciated bilaterally. The patient is not able to report how long her legs have looked like this but her husband states that they have progressed to this point over the past few years. Though this was not the primary diagnosis for the patient’s admission, the patient’s physical exam was indicative of stasis dermatitis and lipodermatosclerosis. She was managed with leg elevation, emollients, washing with warm water without soap or irritants. Additional therapy and dermatology follow-up were recommended as well as the potential need to switch from amlodipine to another anti-hypertensive, however; this remains at the discretion of the patient and her primary care physician.
Risk factors for stasis dermatitis are increasing age, female sex, obesity, varicose veins, history of deep vein thrombosis or thrombophlebitis, amlodipine, as well as diseases causing increased permeability like heart failure, diabetes, and hepatic or nephrotic diseases. Venous hypertension in the setting of chronic venous insufficiency leads to increased hydrostatic pressure and extravasation of erythrocytes. Characteristic red-brown/verrucous pigmentary changes occur as a result of chronic inflammation as well as hemosiderin deposition within the dermis. Initial lesions typically present in the perimalleolar region as a sharply marginated, erythematous, crusted plaque but may progress over time with superimposed lichenification, exudate, ulceration, and development of lipodermatosclerosis. Lesions are most often bilateral, but can occasionally be unilateral, and can be accompanied by pruritis, dull-aching pain, feelings of heavy/tight limbs, and pitting edema which improves with elevation. In this instance the patient also has lipodermatosclerosis which presents with the characteristic thick, hard, contracted skin that gives the leg the appearance of an “inverted champagne bottle”. This is associated with chronic venous insufficiency and obesity as well and is a form of panniculitis resulting from chronic inflammation and hypoxia, fat degeneration, and fibrosis. [3] For both conditions diagnosis is typically clinical and biopsy is not recommended due to poor healing and low-yield histopathology. The presence of swelling and the compromised skin barrier increases the risk of complications like cellulitis, allergic contact dermatitis, lymphangitis, and ulceration. Treatment begins by addressing chronic venous insufficiency which involves leg elevation, daily exercise, and compression and/or ablative therapy. Fibrinolytic therapy has also been suggested for the treatment of lipodermatosclerosis in patients unable to tolerate compression therapy. Skin care involves gentle cleansing, use of bland emollients, and in some instances the use of mild to high-potency topical steroids.
References:
- Usatine, R. P., & Riojas, M. (2010). Diagnosis and Management of Contact Dermatitis. American Family Physician, 249-255.
- Fatourechi, V. (2005). Pretibial Myxedmea: Pathophysiology and Treatment Options. American Journal of Clinical Dermatology, 295-30
- Miteva, M., Romanelli, P., & Kirsner, R. S. (2010). Lipodermatosclerosis. Dermatologic Therapy, 375-388.
Image Challenge: Week 20 - Friday, August 21, 2020

A 67-year-old male with a past medical history of squamous cell carcinoma of his right eyelid presented with multiple rough, scaly, red plaques on the top of his head, both arms and dorsal hands for the past year. Since his retirement, he spends his time fishing and doing outdoor projects. He endorses occasional itching but denies any change in size. Which of the following is the most likely diagnosis?
A) Actinic keratosis
B) Basal cell carcinoma
C) Keratoacanthoma
D) Seborrheic keratosis
E) Squamous cell carcinoma
Correct Answer: A) Actinic keratosis
Incorrect Answers:
B) Basal cell carcinoma (BCC), an abnormal growth of basal cells, generally presents as a pearly, pink papule with telangiectasias on sun-exposed areas of the skin, such as the face, neck, forearms and hands. Moreover, multiple clinicopathologic variants including nodular, infiltrative and morpheaform exist. Sun exposure is the major risk factor. On histology, nests of basaloid cells can be seen with peripheral palisading, fibromyxoid stroma and clefts. The main treatment of choice is surgical excision, most preferably Mohs micrographic surgery. Fortunately, this malignant neoplasm has a low metastasis rate and excellent prognosis with surgery alone.
C) Keratoacanthoma, a variant of squamous cell carcinoma, is a skin lesion found commonly on sun-damaged skin areas. It generally presents as a round, erythematous nodule filled with keratin. Moreover, keratoacanthoma are characterized by rapid growth over days to weeks. Histologically, there is a crateriform nodule composed of well-differentiated keratinocytes, central keratin plug, and eosinophilic inflammation. Some lesions demonstrate spontaneous involution; however, definitive therapy is recommended. Surgical excision or curettage is typically performed to avoid local destruction, recurrence, or metastasis (though rare).
D) Seborrheic keratosis (SK), colloquially known as ‘wisdom spots’, is a benign lesion frequently seen in older people. SKs classically appear as tan-brown, waxy, stuck-on papules occurring on any part of the body. SKs are generally diagnosed clinically, but if needed, biopsy can be done. On histology, SKs present as hyperkeratosis with pseudo-horn cysts and flat base. Treatment is not necessary, but if desired, SKs can be removed using cryotherapy, curettage, or laser. All these methods of removal may result in pigmentation loss of the area, and spontaneous remission is common.
E) Squamous cell carcinoma (SCC), an abnormal growth of squamous keratinocytes, manifests as hyperkeratotic erythematous plaques, patches, or nodules with or without ulceration on sun-exposed areas of the skin, such as the face, neck, and dorsal extremities. Histologically, differentiated keratinocytes with keratin pearls confined to the epidermis are considered SCC in situ, and those invading into the dermis are known as invasive SCC. The main treatment is surgical excision.
Actinic Keratosis (AK)
Surav Man Sakya, BS; Alexandra Flamm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD
A 67-year-old male with a past medical history of squamous cell carcinoma of his right eyelid presented with multiple rough, scaly, red plaques on the top of his head, both arms and dorsal hands for the past year. Since his retirement, he spends his time fishing and doing outdoor projects. He endorses occasional itching but denies any change in size. On physical exam, multiple rough, scaly, red plaques on the top of his head and arms were observed. The rest of skin exam did not show any lesions of concern. A shave biopsy revealed basal layer atypia with finger-like projections into the dermis and overlying parakeratosis. Based on his history, exam and pathology report, actinic keratosis was diagnosed. No other intervention was recommended except for continued self-monitoring for any changes.
Actinic keratoses (AKs) are rough, scaly, red papules or plaques that typically develop from chronic sunlight/UVB exposure, aging and decreased immune system function. They more commonly affect fair to light-skinned individuals and are frequently seen in older people. These lesions are commonly found on sun-exposed areas of the skin including the ears, nose, cheeks, forehead and scalp. While AKs are often referred to as ‘precancerous’ lesions, the rate of malignant transformation into SCC is less than 0.1%. [1] Although AKs can be clinically diagnosed, biopsy can differentiate AKs from SCC. On histology, AKs have atypical basal layer in the epidermis with budding and finger-like projections into the dermis. Furthermore, overlying parakeratosis with hyperkeratosis can be seen. In contrast, on histology, cutaneous SCCs present as differentiated keratinocytes with keratin pearls invading different skin layers. AKs, the most common adult skin disease, are often found during skin examination with an estimated prevalence ranging from 1% to 44%. [2] AK can be observed for concerning changes or treated with cryotherapy, excision, or topical creams, such as 5-FU, imiquimod, or ingenol mebutate. For prevention of AKs, patients are advised to protect themselves from ultraviolet light by applying (and reapplying) SPF 30+ or greater sunscreen and/or wear sun-protective hat and clothing. [3]
References:
- Actinic Keratosis. 2015. Retrieved from https://dermnetnz.org/topics/actinic-keratosis/
- Berry K, Butt M, and Kirby JS. (2017). “Influence of Information Framing on Patient Decisions to Treat Actinic Keratosis”. JAMA dermatology, 153(5): 421–426.
- Alikhan A and Hocker TLH. Review of Dermatology. Elsevier - Health Sciences Division; 2017.
Image Challenge: Week 19 - Friday, August 14, 2020

A 25-year-old female with no significant past medical history presented with a dark-brown, mammillated, oval-shaped patch with hair strands under her left axilla. She has had the mole since birth, and denies any changes in size, shape or color. She does not have any family history of skin cancer. Which of the following is the most likely diagnosis?
A) Congenital melanocytic nevus
B) Dermal melanocytosis
C) Lentigo simplex
D) Melanoma
E) Solar lentigo
Correct Answer: A) Congenital melanocytic nevus
Incorrect Answers:
B) Dermal melanocytosis, colloquially known as a ‘Mongolian spot’ presents as a grey-blue patch on the lumbosacral region predominately in Asians and African Americans. This benign condition is self-resolving without malignant potential. On histology, melanocytes are distributed in the lower 2/3 of the dermis parallel to epidermis with mild increase in melanocyte density.
C) Lentigo simplex is a well-demarcated, brown to black macule that can occur at any age and on any part of the body. Although they may resemble melanomas, they are generally considered benign lesions unrelated to sun exposure. On histology, hyperpigmentation of the basal layer, mild increase in melanocyte density and elongation of the rete ridges are observed. However, multiple lentigines found on the body may require further evaluation because they are associated with, but not limited to, Peutz-Jeghers and xeroderma pigmentosa.
D) Melanoma, a malignant skin cancer from uncontrolled proliferation of melanocytes, generally presents as a dark-brown to black, ‘ugly duckling’ mole with atypical features. The ABCDE criteria (Asymmetry, Border (irregular), Color (variations in pigmentation), Diameter (>6 mm) and Evolving (changes in size, shape, or color) is assessed for all suspicious skin lesions. However, full-thickness excision biopsy is the best confirmatory test. Moreover, melanoma can be divided into four subtypes by predilection sites, morphology and depth of invasion. Although UV radiation exposure is the biggest risk factor, there may be a genetic component, such as CDKN2A mutations.
E) Solar lentigo, colloquially called ‘sun spots’ refers to multiple hyperpigmented macules and patches on sun-exposed areas of the skin, such as the face, neck, forearms and hands. They more commonly affect fair to light-skinned individuals and are frequently seen in older people. Histologically, elongated bulbous rete ridges with hyperpigmentation can be seen. Although they are generally benign, one treatment option is laser therapy.
Congenital Melanocytic Nevus
Surav Man Sakya, BS; Alexandra Flamm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD
A 25-year-old female with no significant past medical history presented with a dark-brown, mammillated, oval-shaped patch with hair strands under her left axilla. She has had the mole since birth, and denies any changes in size, shape or color. She does not have any family history of skin cancer. On physical exam, a 20 x 5 mm, dark-brown, oval-shaped patch with hair growth was observed on her left axilla. The rest of skin exam was unremarkable without evidence of satellite lesions. Based on her history and exam, congenital melanocytic nevus was diagnosed. No intervention was recommended except for continued self-monitoring for any changes.
Congenital melanocytic nevi appear in various sizes throughout the body during the first year of life. Although the nevi may darken in color and develop concerning proliferative nodules mimicking melanoma over time, the size is considered the most important malignancy factor. More specifically, large nevi (>20 cm) have the greatest malignant potential during the first decade of life. In addition, hair growth from the mole indicates intact hair follicles, and thus the nevus is less concerning for malignancy. Furthermore, congenital melanocytic nevi must be distinguished from neurocutaneous melanocytosis/melanosis, which can appear as a large congenital nevus on posterior axial region or as multiple satellite lesions. These are associated with melanocyte proliferation within the leptomeninges or brain parenchyma, and thus warrant further testing, such as MRI within the first year of life. On histology, compound or intradermal proliferation of melanocytes extending into vessels and adnexal structures may be seen. No intervention is required for small- (<1.5 cm) and medium-sized (1.5 - 19.9 cm) nevi unless for cosmetic reasons. Large nevi may be surgically resected after six months of age and may require continuous monitoring via serial examinations or biopsies. [1]
Reference:
1. Alikhan A, Hocker TLH. Review of Dermatology. Elsevier - Health Sciences Division; 2017.
Image Challenge: Week 18 - Friday, August 7, 2020

A 67-year-old male presents to clinic with an enlarging growth on his back. He has a personal history of basal cell carcinoma but denies a family history of skin cancer. The patient states he noticed the spot on his back a few months ago and that it has increased in size and thickness. He states it is itchy and occasionally it flakes off but denies any bleeding. What is the most likely diagnosis?
A) Keratoacanthoma
B) Psoriasis
C) Seborrheic keratosis
D) Tinea corporis
E) Verruca vulgaris
Correct Answer: C) Seborrheic keratosis
Incorrect Answers:
A) Keratoacanthoma is a skin lesion that appears in sun damaged skin and is a variant of squamous cell carcinoma. It presents as a round erythematous nodule filled with keratin. They are characterized by phases of rapid growth, lesion stability, and often spontaneous involution. Diagnosis is made via biopsy. They are managed surgically as they can be locally destructive. [1]
B ) Psoriasis is a chronic inflammatory skin condition that can start at any age with peaks at ages 15-25 and 50-60. It is classified as an immune mediated inflammatory disease and tends to persist lifelong with fluctuating severity. Unlike seborrheic keratosis, it classically presents as symmetrically distributed red plaques with silver scale on the scalp, elbows, or knees. It is diagnosed clinically. Treatment involves topical steroids, phototherapy, systemic treatments, or biologics depending on severity. [2]
D) Tinea corporis is an infection of the trunk, legs, or arms with a dermatophyte fungus. Unlike seborrheic keratosis, it presents as round or oval scaly patches with characteristic central clearing. Diagnosis is confirmed via microscopy and culture of skin scrapings. Treatment is generally with topical antifungals. Systemic antifungals may be used if the symptoms persist. [3]
E) Verruca vulgaris, also known as common warts, are keratotic lesions caused by human papillovirus (HPV). They present as verrucous papules with characteristic pinpoint black dots on the surface. They are most common on the fingers, elbows, and knees. Treatment options include topical applications of keratolytics like salicylic acid, occlusion with duct tape, or cryotherapy.
Seborrheic Keratosis
Sarah Kitts, BS; Alexandra Flamm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD
A 67-year-old male presents to clinic with an enlarging growth on his back. He has a personal history of basal cell carcinoma but denies a family history of skin cancer. The patient states he noticed the spot on his back a few months ago and that it has increased in size and thickness. He states it is itchy and occasionally it flakes off but denies any bleeding.
Seborrheic keratosis are common benign lesions that appear during adult life and are a sign of skin aging. It is estimated that over 90% of adults over the age of 60 have one or more of them. They occur in males and females, and can begin to be seen starting in the 30s or 40s. They can arise on almost any area of the skin, though they usually spare the palms and soles. They are highly variable in appearance but classically have a waxy, stuck on appearance. Seborrheic keratosis can be diagnosed clinically. On dermoscopy, there are often milia like cysts noted on the surface. While seborrheic keratosis are harmless, they can be removed with locally destructive therapies, such as cryotherapy. [4]
References:
1. Oakley, A (1999). Keratoacanthoma.
Retrieved from https://dermnetnz.org/topics/keratoacanthoma/
2. Oakley, A (2014). Psoriasis. Retrieved from https://dermnetnz.org/topics/psoriasis/
3. DermNetNZ (2013). Tinea Corporis.
Retrieved from https://dermnetnz.org/topics/tinea-corporis/
4. Oakley, A (2016). Seborrheic Keratosis.
Retrieved from https://dermnetnz.org/topics/seborrhoeic-keratosis/
Image Challenge: Week 17 - Friday, July 31, 2020

A previously healthy 3-year-old girl presented to the emergency department with fever and rash. She has no history of skin disorder and is meeting all developmental milestones. She is up to date on immunizations. Two days ago, the patient developed a low-grade fever and decreased appetite. Yesterday, a pruritic rash consisting of pink papules developed on her trunk, then spread to her upper and lower extremities, and the rash later became vesicular. This morning, the patient’s father noticed a new group of vesicles on her legs. She is irritable and scratches her rash constantly. She does not have any lesions in her mouth. What is the most likely diagnosis?
A) Eczema herpeticum (HSV-1)
B) Hand-foot-and-mouth disease (coxsackievirus)
C) Roseola (HHV-6)
D) Scabies (Sarcoptes scabiei)
E) Varicella (VZV)
Correct Answer: E) Varicella (VZV)
Incorrect Answers:
A) Eczema herpeticum is caused by HSV-1 or HSV-2 on areas of skin affected by atopic dermatitis, which can cause painful vesicular rash, fever, and dissemination to other parts of the body (e.g. CNS). This patient does not have a history of atopic dermatitis.
B) Hand-foot-and-mouth disease is caused by enteroviruses (e.g. coxsackievirus). It presents with vesicular, pruritic exanthem on the hands and feet including the palms and soles and an oral enanthem of ulcers in the mouth. This patient does not present with oral enanthem.
C) Roseola is caused by human herpesviruses 6 and 7 and presents with high fever followed by a diffuse maculopapular rash, sparing the face after the fever subsides. This patient has vesicular lesions that do not coincide with this presentation.
D) Scabies is caused by Sarcoptes scabiei mite and classically presents as a pruritic, erythematous, papular rash in the interdigital web spaces, flexor surfaces of the wrist, and periumbilical area. This patient presents with fever and diffuse maculopapular rash.
Varicella Zoster in Children
Julie Hong, BS; Alexandra Flamm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD
A previously healthy 3-year-old girl presented to the emergency department with fever and rash. She has no history of skin disorder and is meeting all developmental milestones. She is up to date on immunizations. Two days ago, the patient developed a low-grade fever and decreased appetite. Yesterday, a pruritic rash consisting of pink papules developed on her trunk, then spread to her upper and lower extremities, and the rash later became vesicular. This morning, the patient’s father noticed a new group of vesicles on her legs. She is irritable and scratches her rash constantly. She does not have any lesions in her mouth. Temperature is 100.4 F and heart rate is 100 bpm. Physical exam shows erythematous vesicles and crusted papules. Her mucous membranes are normal. Based on the clinical presentation, the patient was diagnosed with a mild case of varicella, also known as chickenpox, and received supportive care to control her fever and pruritus. She was discharged from the hospital after 2 days.
Varicella-zoster virus (VZV) can lead to two different forms of infections: chickenpox in children and shingles in adults. The incidence of chickenpox in children in the U.S. has declined greatly due to universal vaccination. However, because the two doses of varicella vaccinations are administered at age 1 and 4, breakthrough infection is possible in children who have received only a single dose of vaccine, as in this 3-year-old patient who is up to date on her immunizations but did not receive her second dose of VZV vaccine [1, 2]. In this population of patients, breakthrough infections are generally mild with lower fever and fewer skin lesions. About 2 weeks after exposure to airborne particles, patients with chickenpox develop fever and malaise followed by intensely pruritic, vesicular rash involving the trunk, face, and extremities within 24 hours. New “crops” of vesicles can appear daily for over a week and then become pustular and crust over, healing at different stages. Chickenpox is highly contagious, but generally self-limiting, and immunocompetent patients do not require any antiviral therapy. Rarely, it can cause superimposed bacterial skin infection, cerebellar ataxia, or pneumonia.
Reference:
- Cenoz MG, Martínez-Artola V, Guevara M, Ezpeleta C, Barricarte A, Castilla J. Effectiveness of one and two doses of varicella vaccine in preventing laboratory-confirmed cases in children in Navarre, Spain. Hum Vaccin Immunother. 2013;9(5):1172-1176. doi:10.4161/hv.23451
- Thomas CA, Shwe T, Bixler D, et al. Two-dose varicella vaccine effectiveness and rash severity in outbreaks of varicella among public school students. Pediatr Infect Dis J. 2014;33(11):1164-1168. doi:10.1097/INF.0000000000000444
Image Challenge: Week 16 - Friday, July 24, 2020

28-year-old male with a past medical history of asthma and allergic rhinitis presents with intense itching between his fingers. The area weeps and bleeds after itching. It has been occurring since he was in high school and is worse during winter but is around all year-round. Eucerin cream and hot water on the hand helps with itching but nothing takes it away. There is no one else in his home wih similar symptoms and the patient has no family history of skin conditions. What is the most likely diagnosis?
A) Atopic Dermatitis
B) Ichthyosis Vulgaris
C) Palmar Psoriasis
D) Scabies
E) Tinea manuum
Correct Answer: A) Atopic Dermatitis
Incorrect Answers:
B) Ichthyosis vulgaris, characterized by excessive dry, scaly skin, results from mutations in the gene encoding the protein filaggrin. It generally effects a large area of the body and will first appear from the ages of 2 months to 5 years with symptoms worsen up to puberty. [1]
C) Psoriasis is a chronic inflammatory skin condition characterized by clearly defined, red and scaly plaques (thickened skin). It can first appear at any age, including childhood, with peak onset at 15-25 and 50-60 years. About 1/3 of patients have a family history of psoriasis. Psoriasis is an immune mediated condition that can be aggravated by a number of different factors such as infections, smoking and stress. [2]
D) Scabies is a very itchy rash caused by a parasitic mite that burrows into the skin surface, often in the finger web space. The mites can be transmitted from person to person in close contact with each other such as in families, retirement homes, and prisons. Often a burrow is seen on physical examination. [3]
E) Tinea manuum is an infection of 1 or both hands with a dermatophyte infection. It is an acute inflammatory rash with a raised red boarder with a central clearing and overlying scale. It causes itching and burning. Diagnosis is made clinically and can be aided with a KOH prep. [4]
Atopic Dermatitis
Deep Patel, BS; Alexandra Flamm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD
A 28-year-old male with a past medical history of asthma and allergic rhinitis presents with intense itching and skin thickening between his fingers. The area weeps and bleeds after itching. It has been occurring since he was in high school and is worse during winter but is around all year-round. Eucerin cream and hot water on the hand helps with itching but nothing takes it away. There is no one else in his home with similar symptoms and the patient has no family history of skin conditions. Physical exam reveals a crusted lichenified patch on the right lateral third finger. Diagnosis of atopic dermatitis was made clinically and prescribed triamcinolone to be used to cure lesions then intermittently during flares.
Atopic dermatitis, also known as eczema, is a chronic, itchy skin condition that is very common in children but may occur at any age. Atopic dermatitis is a part of the atopic triad and is usually associated with asthma and allergic rhinitis. Atopic dermatitis arises because of a complex interaction of genetic and environmental factors. These include defects in skin barrier function making the skin more susceptible to irritation by soap and other contact irritants, the weather, temperature and non-specific triggers. It is impossible to predict whether eczema will improve by itself or not in an individual. Reduction of exposure to trigger factors, regular emollients (moisturization) and intermittent topical steroids is common first line treatment. In more severe cases, management can include topical calcineurin inhibitors, phototherapy, immunosuppressive agents or biologic therapy (Dupilumab).
Reference(s):
- Lee N. Ichthyosis Vulgaris. https://dermnetnz.org/topics/ichthyosis-vulgaris/. Accessed July 20, 2020.
- Oakley A. Psoriasis. https://dermnetnz.org/topics/psoriasis/. Accessed July 20, 2020.
- Oakley A. Scabies. https://dermnetnz.org/topics/scabies/. Accessed July 20,2020.
- Tinea manuum. https://dermnetnz.org/topics/tinea-manuum/. Accessed July 20, 2020.
- Stanway A. Atopic Dermatitis. https://dermnetnz.org/topics/atopic-dermatitis/. Accessed July 20, 2020.
Image Challenge: Week 15 - Friday, July 17, 2020

20-year-old male with no significant past medical history presents with a 6-month history of left toenail discoloration. It is specifically confined to the left 4th and 5th toes, with no involvement of other digits on the left or the right foot. He is a tennis player and plays consistently every day, but this is the first time he has ever had an issue like this. He noticed the discoloration suddenly while taking off his socks and shoes after a practice. He denies any inciting events, triggers, or recent travel that he thinks may have caused this. He describes the toes as a “weird color” and denies other issues with the foot such as tenderness or itchiness. The color has not changed and has not gotten better or worse over the last 6-months. He has not tried anything at home because he is not sure what to do for them and is very embarrassed. On exam, the left 4th and 5th toenails are thickened and discolored with overlying scale, particularly at the nail bed. Onycholysis is also present in the 5th nail. What is the most likely diagnosis?
A) Lichen planus
B) Nail trauma
C) Onychogryphosis
D) Onychomycosis
E) Psoriasis
Correct Answer: D) Onychomycosis
Incorrect Answers:
A) Lichen Planus is a chronic inflammatory condition of the skin and mucosal surfaces normally affecting adults >40 years old. While most commonly affecting the mouth, a small percent of patients have nail involvement. This disorder is mediated by T cells which attack a protein within the skin and keratinocytes in response to multiple triggers. These include stress, trauma, localized skin disease, viral infections, allergies, drugs, and graft versus host disease. When involving the nails, there is thinning of the nail plate with the appearance of grooves and ridges. If left untreated, it can progress to cause cuticle damage and disappearance of the nail. While this patient has some changes at the nail plate, his nails are exhibiting more thickening than the thinning seen in lichen planus [3].
B) Nail trauma may lead to fracturing and subsequent destruction of the nail plate. The plate then tends to become yellow and opaque, associated with onycholysis or detachment from the nail bed. Most of the time, nail trauma is associated with subungual hemorrhage which appears as a reddish, purple, brown, or black discoloration underneath the nail plate. Opposed to 6 months without improvement, as in our patient, normal nail growth occurs after trauma leading to a clear proximal margin in the nail plate within a few weeks of the injury [5].
C) Onychogryphosis is a disorder of slow nail plate growth leading to an opaque, yellow-brown thickening of the nail plate with increased curvature. This disorder can be congenital or acquired, and is seen most commonly in the elderly or those with poor personal hygiene. It has been associated with psoriasis, syphilis, gout, poor circulation, diabetes, injury, and bunions. After the initial trigger, the nail plate undergoes significant hypertrophy at the proximal matrix leading to elongation of the nail with increased curvature, giving the nail a “ram’s horn” appearance. This condition, if left untreated, can be associated with secondary onychomycosis. While our patient has the classic discoloration, his nail thickening is not as pronounced as what is normally seen in onychogryphosis. Nail clippings and culture should be taken in order to fully distinguish the two conditions [1].
E) Nail Psoriasis is a condition most commonly associated with chronic plaque psoriasis or psoriatic arthritis but can be an isolated disorder precipitated by trauma. This condition arises in the nail matrix and appears as scaly plaques on the dorsum of the hands or feet along with nail plate thickening, pitting, leukonychia, onycholysis, and hyperkeratosis. It can also be associated with yellow-red discoloration (“salmon patch”), splinter hemorrhages, transverse ridges, and a pustular eruption of the nail bed or matrix. While this patient has some scaling and hyperkeratosis of the nails, there are no secondary nail features present that would point toward a diagnosis of psoriasis [2].
Onychomycosis
Morgan Chambers, BS; Alexandra Flamm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD
20-year-old male with no significant past medical history presents with a 6-month history of left toenail discoloration. It is specifically confined to the left 4th and 5th toes, with no involvement of other digits on the left or the right foot. He is a tennis player and plays consistently every day, but this is the first time he has ever had an issue like this. He noticed the discoloration suddenly while taking off his socks and shoes after a practice. He denies any inciting events, triggers, or recent travel that he thinks may have caused this. He describes the toes as a “weird color” and denies other issues with the foot such as tenderness or itchiness. The color has not changed and has not gotten better or worse over the last 6-months. He has not tried anything at home because he is not sure what to do for them and is very embarrassed. On exam, the left 4th and 5th toenails are thickened and discolored with overlying scale, particularly at the nail bed. Onycholysis is also present in the 5th nail. Based on clinical exam and features, the patient was diagnosed with onychomycosis. The patient was educated on ways to maintain proper foot hygiene, including keeping the feet dry and putting on clean socks/shoes after tennis practice. Meanwhile, OTC topical antifungal ointment/cream was recommended.
Onychomycosis, a fungal infection of the nail, is caused by dermatophytes, yeasts, or molds. This infection can present in many different patterns on any toenail or fingernail, but most commonly on the first of fifth nail. Classic features include discoloration at one side of the nail, scaling, onycholysis with crumbling of the free edge, and destruction of the nail plate. While able to be diagnosed clinically, it is confirmed with nail clippings and scrapings with further microscopy and culture. Treatment of onychomycosis can be done with topical antifungal agents; however oral antifungals are usually required to fully cure it. Other new-found methods of treatment are lasers, photodynamic therapy, or ultrasound to enhance the delivery of drugs to the nail plate [4]
References:
- Nakao, A.; Oakley, A. (2019). Retrieved from https://dermnetnz.org/topics/onychogryphosis/
- Ngan, V. (2003). Oakley, A. (2016). Nail psoriasis. Retrieved from https://dermnetnz.org/topics/nail-psoriasis/.
- Oakley, A. (1997). Updated 2015. Lichen planus. Retrieved from https://dermnetnz.org/topics/lichen-planus/.
- Oakley, A. (2003). Fungal nail infections. Retrieved from https://dermnetnz.org/topics/fungal-nail-infections/.
- Phillips, M.; Oakley, A. (2020). Subungual haemorrhage. Retrieved from https://www.dermnetnz.org/topics/subungual-haemorrhage/#:~:text=The%20trauma%20may%20destroy%20or,plate%20and%20the%20nail%20bed.
Image Challenge: Week 14 - Friday, July 10, 2020
Click to download explanation with photos
21-year-old female presented to clinic with a new spot on her leg. She has seasonal allergies and a history of an anterior cruciate ligament tear. She previously used tanning beds for 2-3 months each year in high school. She no personal or family history of skin cancer. She noticed the spot on her leg a few weeks ago when she cut it when she was shaving. She has done this a couple more times since then. Otherwise, it is not painful or itchy. It has not grown or changed over this time. She has tried over-the-counter salicylic acid since she thought it was a wart, but noticed only skin redness and peeling without any improvement. What is the most likely diagnosis?
A) Bacterial folliculitis
B) Dermatofibroma
C) Keratoacanthoma
D) Molluscum contangiosum
E) Verruca vulgaris
Correct Answer: B) Dermatofibroma
Incorrect Answers:
A) Bacterial folliculitis, an inflammation of the hair follicles often cause by Staphylococcus aureus, presents as a tender red spot often with a pustule. Unlike dermatofibroma, there are typically multiple lesions. They can be superficial or deep and can affect anywhere there are hairs including the chest, back, buttocks, arms, and legs. [1]
C) Keratoacanthoma is a skin lesion that appears in sun damaged skin and is a variant of squamous cell carcinoma. It presents as a round erythematous nodule filled with keratin. They are characterized by phases of rapid growth, lesion stability, and spontaneous involution. Diagnosis is made via biopsy. They are managed surgically as they can be locally destructive. [2]
D) Molluscum contagiosum is a common viral skin infection that appears as localized clusters of umbilicated epidermal papules. Unlike dermatofibroma, there are typically multiple lesions. It is caused by a DNA poxvirus. It is classically seen in children under ten years old or immunocompromised adults. [3]
E) Verruca vulgaris, also known as common warts, are keratotic lesions caused by human papillovirus (HPV). They present as verrucous papules with characteristic pinpoint black dots on the surface. They are most common on the fingers, elbows, and knees.
Dermatofibroma
Sarah Kitts, BS; Alexandra Flamm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD
Dermatofibromas are common benign fibrous nodules that most often arise on the skin of the lower legs. They occur in people of all ages and are more common in women than men. They appear as pink to light brown, firm nodules that characteristically dimple when the skin is pinched. The lesions are made up of proliferating fibroblasts. Because they are raised, they may be traumatized, often by a razor. Dermatofibromas can be diagnosed clinically. On dermatoscopy there is a central white area surrounded by a faint pigment network. Dermatofibromas are harmless and rarely cause symptoms. [4]
Reference(s):
- Oakley, A (2014). Folliculitis. Retrieved from https://dermnetnz.org/topics/folliculitis/
- Oakley, A (1999). Keratoacanthoma. Retrieved from https://dermnetnz.org/topics/keratoacanthoma/
- Oakley, A (1997) Vanousova, D (2015). Molluscum contagiosum. Retrieved from https://dermnetnz.org/topics/molluscum-contagiosum/
- Oakley, A (2016) Dermatofibroma. Retrieved from https://dermnetnz.org/topics/dermatofibroma/
Image Challenge: Week 13 - Friday, July 3, 2020

Two-month-old baby boy born full-term is seen in clinic for a growth on the left cheek. Mom reports it appeared on the eighth day of life and has grown larger since then. It has never ulcerated, bled, or caused him any problems. Baby appears well nourished, well developed, and in no distress. On the left cheek, there is a 2.5 cm ovoid, red vascular plaque with well demarcated boarders and no ulcerations or crusts. What is the most likely diagnosis?
A) Angiosarcoma
B) Capillary vascular malformation
C) Dermatofibroma
D) Infantile Hemangioma
E) Lipoma
Correct Answer: Infantile Hemangioma
Incorrect Answers:
A) Angiosarcoma, an uncommon and aggressive malignant tumor that arises from endothelial cells, is frequently found in skin and soft tissues but can also originate in the liver, breast, spleen, bone, or heart. Cutaneous angiosarcomas start as an ill-defined bruise and then elevate into larger nodules and plaques that commonly bleed and ulcerate. These tumors are much more common in older adults, commonly with chronic lymphedema, history of radiotherapy, or exposure to agents such as arsenic and vinyl chloride. [1]
B) Capillary vascular malformation arise from malformed dilated blood vessels in the skin. They are non-cancerous and their size can vary tremendously, ranging from a small dot to affecting a whole limb. Baby is born with blotches of red or purple skin discoloration rather than developing them after birth, unlike infantile hemangiomas which appear shortly after birth. [2]
C) Dermatofibroma, a common benign fibrous nodule that is commonly on the skin of the lower legs. They occur at all ages and in people of every ethnicity. They appear as a pink to light brown, firm nodule that dimples when the skin is pinched. They are a result of proliferated fibroblasts, unlike infantile hemangiomas which is due to proliferated endothelial cells. [3]
E) A lipoma is a non-cancerous tumor that is made up of fat cells. It is slow growing and is very common. They are flesh colored nodules and they tend to develop in adulthood and are most noticeable during middle age. [4]
Infantile Hemangiomas
Deep Patel, BS; Alexandra Flamm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD
Two-month-old baby boy born full-term is seen in clinic for a growth on the left cheek. Mom reports that it appeared on the eighth day of life and has grown larger since then. It has never ulcerated, bled, or caused him any problems. Baby appears well nourished, well developed, and in no distress. On the left cheek, there is a 2.5 cm ovoid, red vascular plaque with well demarcated boarders and no ulcerations or crusts. The diagnosed of an infantile hemangioma was made clinically and was treated with propranolol 2 mg oral solution twice per day.
Infantile hemangioma is a benign proliferation of endothelial cells that develops shortly after birth. Over 80% of infantile hemangiomas occur on the head and neck area. They have a characteristic growth and involution phase. Typically, growth phase occurs from birth to three to six months, where lesion grows rapidly and then stabilizes. Involution phase, where lesion shrinks, may take years. Because infantile hemangiomas are likely to improve or regress completely with time, there is no need for specific treatment in most cases but should be considered if lesions are very large, ulcerated, impairing vision, hearing, breathing or feeding, or they fail to resolve by school age. Propranolol is treatment of choice for troublesome hemangiomas. Topical beta-blockers such as timolol can be used off-label for small superficial hemangiomas. [5]
Reference(s):
- Ngan, V (2005) Elghblawi, E (2017). Angiosarcoma. Retrieved from https://dermnetnz.org/topics/angiosarcoma/
- Ngan, V (2005) Oakley, A (2014). Capillary vascular malformation. Retrieved from https://dermnetnz.org/topics/capillary-vascular-malformation/
- Oakley, A (2016). Dermatofibroma. Retrieved from https://dermnetnz.org/topics/dermatofibroma/
- Ngan, V (2003).Lipoma and liposarcoma. Retrieved from https://dermnetnz.org/topics/lipoma-and-liposarcoma/
- Oakley, A (2012). Infantile proliferative haemangioma. Retrieved from https://dermnetnz.org/topics/infantile-haemangioma/
Image Challenge: Week 12 - Friday, June 26, 2020

A 55-year-old female with a history of Darier’s Disease presents to clinic with progressively worsening “bumps” on her hands. The patient reports she has had these bumps “for years” but they seem to be growing in number and size the past few months. She describes these areas as tender but denies any pruritis or other symptoms. She notes similar lesions on both elbows, and the bottom of her right foot. The patient also describes chronic pain and swelling in the hands bilaterally, especially within the metacarpophalangeal (MCP) joints. Physical exam is notable for pink/purple soft nodules on the PIP, DIP, and MCP joints, ulnar deviation of all digits, with tenderness to palpation the MCP joints of the right hand and erythronychia and trachyonchia of all fingernails. Hyperkeratotic papules, consistent with her history of Darier’s disease, are present on the chest but no other rash is present on the body. What is the most likely diagnosis?
A) Dermatomyositis
B) Digital myxoid cysts
C) Eruptive xanthomas
D) Psoriasis
E) Rheumatoid nodules
Correct Answer: E) Rheumatoid Arthritis
Incorrect Answers:
A) Dermatomyositis, an inflammatory myopathy is characterized by symmetric proximal muscle weakness and hallmark cutaneous findings including heliotrope rash (symmetrical erythema of eyelids) and Gottron papules. Unlike this patient’s cutaneous findings, Gottron papules are characterized by violaceous, slightly scaly plaques over the bony prominences of the digits [1].
B) Digital Myxoid Cysts, are characterized as solitary, dome-shaped, cystic nodules on the dorsum hand, and commonly found at the base of the nail. These cysts are most often reported in middle-aged or elderly patients and are slightly more common in females. Multiple cysts on a single finger have been reported but are less common. A wide range of therapies are used to treat these lesions including digital compression, cryotherapy, or surgical excision. [2]
C) Eruptive xanthomas are 1 to 5 mm erythematous to yellow papules that abruptly appear in diffuse pattern. The most common sites of involvement tend to be the extensor surfaces of the extremities and buttocks. This cutaneous finding is highly suggestive of an underlying hypertriglyceridemia, more specifically with serum triglyceride levels exceeding 1500-2000 mg/dL. Eruptive xanthoma histology is characterized by a proliferation of foamy histiocytes and extracellular lipid within the dermis. Treatment consists of correcting the underlying dyslipidemia. [3]
D) Psoriasis is a chronic skin disorder characterized by excessive proliferation of keratinocytes, resulting in the formation of thickened scaly plaques and can manifest as a multisystem inflammatory disorder. Psoriasis often has joint involvement, known as psoriatic arthritis, which is a seronegative inflammatory spondyloarthritis associated with mild-severe psoriasis and joint manifestations. Extraarticular manifestations include scalp lesions, nail dystrophy and intergluteal/perianal lesions. Although this patient presents with abnormal nail findings, they are likely secondary to her existing Darier’s disease considering the absence of typical psoriatic skin findings. When digit involvement is present in psoriatic arthritis, swelling often involves the whole digit (“sausage digit”) rather than swelling around centers of the joint (fusiform) as seen in RA and this patient. Unlike RA and this patient’s presentation, distribution of involved joints tends to be asymmetric and DIP involvement is common. [4]
Rheumatoid arthritis
Xavier Candela, B.S.; Alexandra Flamm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD
A 55-year-old female with a history of Darier’s Disease presents to clinic with progressively worsening “bumps” on her hands. The patient reports she has had these bumps “for years” but they seem to be growing in number and size the past few months. She describes these areas as tender but denies any pruritis or other symptoms. She notes that there are also similar lesions on both elbows. The patient also describes pain and swelling in the hands bilaterally, especially within the metacarpophalangeal (MCP) joints. Physical exam is notable for pink/purple nodules on the proximal interphalangeal (PIP), distal interphalangeal (DIP), and MCP joints, ulnar deviation of all digits, with tenderness to palpation of the MCP joints of the right hand and erythronychia and trachyonchia of all fingernails. Hyperkeratotic papules are present on the chest, but no other rash is present on the body. Based on clinical exam and features, the patient was diagnosed with rheumatoid arthritis. The patient was educated on the condition and started on methotrexate 20mg every 7 days. A discussion also took place of the possibility of starting a TNF-alpha inhibitor in the absence of significant improvement with methotrexate alone. Methotrexate drug levels, serum creatinine, electrolytes and anti-citrullinated peptide were ordered to monitor side effects of therapy and confirm the diagnosis, respectively. Rheumatoid arthritis (RA) is a chronic, inflammatory joint disease characterized by synovial inflammation, which can destroy articular cartilage and juxtaarticular bone. RA has a worldwide prevalence of roughly 5 per 1000 adults and affects 2-3 times more women than men. The disease presents as a polyarticular symmetric disease that involves multiple joints bilaterally, with pain and swelling in the hands and feet. Both small (MCP, PIP) and large joints (elbow, knee) can be affected, but the DIP joints are rarely involved. The diagnosis is based on a combination of history, physical exam findings, and laboratory values. A diagnosis can be made clinically, but serology levels of rheumatoid factor (high sensitivity, low specificity), CRP/erythrocyte sedimentary rate (acute phase reactants), and CCP (low sensitivity, high specificity) can aid in confirming the diagnosis. Advanced RA can display extra articular manifestations include rheumatoid nodules (firm subcutaneous lumps near bony prominences such as elbows as seen in this case). Histologically, rheumatoid nodules display intensely staining eosinophilic necrobiosis surrounded by histiocytes in palisade arrangement. Cardiovascular disease is a common consequence of chronic inflammatory conditions such as RA and is the primary cause of death in this disease. Treatment regimens include rapidly acting anti-inflammatory medications including NSAIDs and glucocorticoids; non-biologic disease modifying anti-rheumatic drug (DMARDs) including hydroxychloroquine, sulfasalazine, and methotrexate; and biologic DMARDs including TNF-alpha inhibitors, IL-1 receptor antagonist anakinra, and IL-6 receptor antagonists tocilizumab. These more aggressive treatment regimens with targeted biologic therapies are best suited to reduce cardiovascular risk [5].
Reference(s):
- Rider, L. (2011). Deciphering the Clinical Presnetations, Pathogenesis, and Treatment of the Idiopathic Inflammatory Myopathies. JAMA. Retrieved from: https://jamanetwork.com/journals/jama/article-abstract/644992
- Patterson, J. 2021. Weeden’s Skin Pathology. Retrieved from: https://www.clinicalkey.com/#!/content/3-s2.0-B9780702075827000149?scrollTo=%23hl0000353
- Bologina, J. (2014). Xanthomas. Dermatology. Retrieved from: https://www-clinicalkey-com.ezaccess.libraries.psu.edu/#!/content/book/3-s2.0-B9780702062759000921?scrollTo=%23top
- Ritchlin, C. (2017) Psoriatic Arthritis. NEJM. Retrieved from: https://pubmed.ncbi.nlm.nih.gov/28273019/
- Aletaha, D. (2018). Diagnosis and Management of Rheumatoid Arthritis: A Review. JAMA Retrieved from: https://jamanetwork-com.ezaccess.libraries.psu.edu/journals/jama/fullarticle/2705192
Image Challenge: Week 11 - Friday, June 19, 2020

A 30-year-old G2P0010 at 37 weeks gestation with a history significant for hypothyroidism presents to the dermatology clinic for evaluation of an acute rash that began one week ago. She first noticed the rash on her thighs then spread to her abdomen. She has never experienced a rash like this before and she has tried to treat it at home with over the counter creams with no relief. The rash is mildly pruritic and she has no pain, burning, or other symptoms. Of note, the patient is currently taking ferrous sulfate, levothyroxine, and a prenatal vitamin. On exam, she was in no acute distress and vitals were stable. There are scattered, pink, dermal papules and plaques on arms, legs, and abdomen within striae. What is the most likely diagnosis?
A) Contact Dermatitis
B) Pemphigoid Gestationis
C) Polymorphous Eruption of Pregnancy
D) Pustular Psoriasis of Pregnancy
E) Scabies
Correct Answer: C) Polymorphous Eruption of Pregnancy
Incorrect Answers:
A) Contact Dermatitis, a skin reaction due to direct contact with a causative agent, which can be acute or chronic. Entities that cause contact dermatitis include, but are not limited to: chemicals, irritants, allergies, etc. This process can occur anywhere on the body, but most commonly is localized to the hands. It tends to appear as red, linear/round/polygonal lesions with associated swelling, lichenification, or fissuring, and can even have associated crusting and/or papules. While atopic eruptions can commonly occur in pregnancy due to the reduction of Th1 cytokines and increase in Th2, this patient’s rash is generalized and heavily involves the abdominal striae. Also, it does not seem to exhibit a particular pattern that would suggest the use of a contact irritant [2, 4].
B) Pemphigoid gestationis, also called herpes gestationis, is a rare autoimmune bullous disease occurring in the 2nd or 3rd trimester of pregnancy caused by circulating IgG1 autoantibodies directed against the bullous pemphigoid antigen. Similar to bullous pemphigoid, the binding of antibodies to the basement membrane leads to a separation of the epidermis and dermis. This condition begins with intense itching which then leads to the eruption of urticarial plaques and papules around the umbilicus. Additionally, unlike this patient, the rash also exhibits tense blisters [4].
D) Pustular psoriasis of pregnancy typically presents in the 3rd trimester but can occur any time. It most commonly appears as erythematous plaques which enlarge from the periphery as the center erodes and becomes crusted. It is located in the flexural areas initially and then spreads, sparing the hands, feet, and face. Unlike this patient, pruritus is normally absent [4].
E) Scabies, a rash caused by the burrowing of Sarcoptes scabiei var. hominis in human skin, most commonly occurs in children and elderly patients. However, it arises in overly crowded populations or those with low socioeconomic status. The resulting rash is a hypersensitivity reaction that occurs 4-6 weeks after initial infestation. It is a generalized rash that is commonly located in the finger web spaces, on palms, wrists, elbows, armpits, buttocks, groin. Morphology tends to vary; however, linear tracks are commonly seen along with erythematous papules on trunk/limbs and vesicles on palms and soles. The rash is associated with intense itch that can persist for several weeks, even after treatment. While this patient had intense itch, her hands, palms, and soles were spared, and she had the most significant involvement of her abdominal striae.
Polymorphous Eruption of Pregnancy
Morgan Chambers, BS; Alexandra Flamm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD
A 30-year-old G2P0010 at 37 weeks gestation with a history significant for hypothyroidism presents to the dermatology clinic for evaluation of an acute rash that began one week ago. She first noticed the rash on her thighs then spread to her abdomen. She has never experienced a rash like this before and she has tried to treat it at home with over the counter creams with no relief. The rash is mildly pruritic, and she has no pain, burning, or other symptoms. Of note, the patient is currently taking ferrous sulfate, levothyroxine, and a prenatal vitamin. On exam, she was in no acute distress and vitals were stable. There are scattered, pink, dermal papules and plaques on arms, legs, and abdomen within striae. Based on clinical exam and features, the patient was diagnosed with Polymorphous Eruption of Pregnancy. The patient was educated on the condition, including that it would not have any effects on the baby and that it should improve in the 4-6 weeks after delivery. Meanwhile, she was prescribed topical triamcinolone cream 0.1% to use over the affected area twice per day for some relief.
Polymorphic eruption of pregnancy is a common, self-limiting pruritic inflammatory disorder that normally arises in the last few weeks of pregnancy. While the exact cause of the condition is not well understood, it is thought that the amount of stretching in the abdomen plays a role as it leads to connective tissue damage which may trigger an inflammatory response. Another theory is that circulating fetal antigens may trigger a maternal immune response, which leads to the eruption. It typically presents as pruritic, erythematous papules within abdominal striae as well as the extremities, chest, and back. Onset is often in the third trimester, especially in the last 5 weeks when skin stretching is greatest, therefore it is also more common in first pregnancies than subsequent pregnancies. It typically lasts 4-6 weeks and resolves within two weeks after delivery. Diagnosis is largely based upon history and clinical examination, with biopsy not being a necessary step. Since this condition is largely self-limited and will resolve after delivery, the goal of treatment is to relieve the patient’s symptoms. Use of mid-to-high potency topical corticosteroids is common, along with chlorpheniramine or loratidine/cetirizine to control itching [1, 4].
References:
- Oakley, A. (1999), Elghblawi, E. (2017). Polymorphic eruption of pregnancy. Retrieved from https://dermnetnz.org/topics/polymorphic-eruption-of-pregnancy/
- Oakley, A. (2012). Contact dermatitis. Retrieved from https://dermnetnz.org/topics/contact-dermatitis/
- Oakley, A. (1997). Updated 2015. https://dermnetnz.org/topics/scabies/
- Pomeranz, M.K. (2018). Dermatoses of pregnancy. UpToDate. Retrieved from https://www.uptodate.com/contents/dermatoses-of-pregnancy#H13.
Image Challenge: Week 10 - Friday, June 12, 2020

A 32-year-old female with uncontrolled diabetes mellites type 2 and Crohn’s disease presents with a large, non-healing, painful ulcer on her left shin. The area started as a pink bump and has evolved into an ulcer over the past year. She is extremely distraught with the appearance of the wound and reports 8/10 pain. Her vitals are stable. There is a 6X3cm well-demarcated deep ulcer with a beefy red, fibrinous base containing visible subcutaneous tissue and a rim of erythema and areas of undermined edges. Dorsalis pedis and posterior tibial pulses are 2+ on her left leg. A biopsy of the ulcer edge showed diffuse dense neutrophil infiltrates in the dermis. Labs were within normal limits and wound culture did not grow any colonies. What is the most likely diagnosis?
A) Arterial Ulcer
B) Ecthyma Gangrenosum
C) Factitious Ulcer
D) Necrotizing Fasciitis
E) Pyoderma Gangrenosum
Correct Answer: E) Pyoderma Gangrenosum
Incorrect Answers:
A) Arterial ulcers are due to inadequate blood supply to an affected area. Patients usually have risk factors that may lead to developing inadequate blood supply, such as diabetes, smoking, hyperlipidemia, hypertension and obesity. These ulcers are generally located at the distal extremities, especially in the lower legs and tops of feet or toes. Unlike this patient, patients with arterial ulcers have decreased dorsalis pedis and posterior tibial pulses, indicating poor perfusion [1].
B) Ecthyma gangrenosum, a cutaneous infection, is most commonly associated with Pseudomonas aeruginosa The lesions initially present as hemorrhagic pustules and later become necrotic (black) ulcers. Unlike this patient, ecthyma gangrenosum usually develops in critically ill and immunocompromised patients [2].
C) Factitious ulcers occur secondary to a patient digging, excoriating, or generally manipulating their own skin. The patient typically lacks concern for how disfiguring the lesions appear and the history generally never adds up to explain the unusual cutaneous findings. This patient is extremely distressed with her condition and has a biopsy result consistent with another diagnosis [3].
D) Necrotizing fasciitis is a very serious bacterial infection of the soft tissue and fascia resulting in destruction of the structures. It can be caused by polymicrobial or a specific bacteria, such as Streptococcus pyogenes, Vibrio vulnificus and Clostridium perfringens. Unlike this patient, necrotizing fasciitis has an incredibly rapid course of action and presents with flu-like symptoms, such as fever, nausea, diarrhea and malaise [4].
Pyoderma Gangrenosum
Deep Patel, BS; Alexandra Flamm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD
A 32-year-old female with uncontrolled diabetes mellites type 2 and Crohn’s disease presents with a large, non-healing, painful ulcer on her left shin. The area started as a pink bump and has evolved into an ulcer over the past year. She is extremely distraught with the appearance of the wound and reports 8/10 pain. Her vitals are stable. There is a 6X3cm well-demarcated deep ulcer with a beefy red, fibrinous base containing visible subcutaneous tissue and a rim of erythema and areas of undermined edges. There is a 1cm central area of exposed muscle. Dorsalis pedis and posterior tibial pulses are 2+ on her left leg. A biopsy of the ulcer edge showed diffuse dense neutrophil infiltrates in the dermis. Labs were within normal limits and wound culture did not grow any colonies. Patient was diagnosed with pyoderma gangrenosum and started oral cyclosporine 200mg twice per day.
Pyoderma gangrenosum presents as an enlarging, painful ulcer and is one of a group of autoinflammatory disorders known as neutrophilic dermatoses. Although about half of those affected by pyoderma gangrenosum have no associated risk factors, inflammatory bowel disease (Crohn’s and Ulcerative colitis), rheumatoid arthritis and monoclonal gammopathy are associated with pyoderma gangrenosum. Most cases of pyoderma gangrenosum are diagnosed after ruling out other causes, such as infection, along with a biopsy that is suggestive of pyoderma gangrenosum. Biopsy typically reveals neutrophilic inflammatory infiltrate at ulcer edge. Due to its autoinflammatory nature, pyoderma gangrenosum is treated with agents, such as systemic corticosteroids, systemic cyclosporine, biologics and other immunomodulators [5].
References:
- Dendale A. Arterial Ulcer. https://dermnetnz.org/topics/arterial-ulcer.
- Duffill M. Ecthyma gangrenosum. https://dermnetnz.org/topics/ecthyma-gangrenosum/.
- Craft N, Fox LP, Goldsmith LA. Factitial Ulcer. https://www.visualdx.com/visualdx/diagnosis/ factitial+ulcer?diagnosisId=52661&moduleId=101.
- Ngan V, Gomez J. Necrotizing fasciitis. https://dermnetnz.org/topics/necrotising-fasciitis/.
- Oakley A. Pyoderma gangrenosum. https://dermnetnz.org/topics/pyoderma-gangrenosum/.
Image Challenge: Week 9 - Friday, June 5, 2020
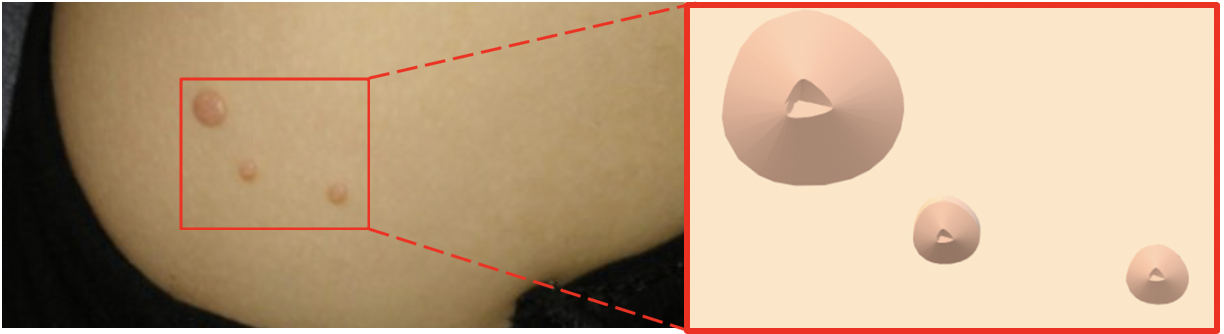
A 5-year-old female with no significant past medical history was brought in by her mother who noticed multiple, painless, skin-colored, pearly papules with central umbilication (inlet on right showing enlarged graphical representation of the papules) on her daughter’s right lower abdomen. She was seen scratching the papules while her mother was dressing her. Her immunizations are up to date. She is at 50th percentile for height and weight. She attends a dance class where another child was reported to have similar lesions. What is the most likely diagnosis?
A. Chickenpox
B. Keratoacanthoma
C. Molluscum Contagiosum
D. Superficial Folliculitis
E. Verruca Vulgaris
Correct Answer: C) Molluscum Contagiosum
Incorrect Answers:
A) Chickenpox, also known as varicella, is caused by the varicella zoster virus and is characterized by pruritic macules, papules, vesicles and crusts in a cephalocaudal distribution. The rash initially presents with vesicles on an erythematous base and later become crusted erosions. Children may experience prodromal symptoms, such as fever, fatigue and myalgias prior to the rash.
B) Keratoacanthoma, a variant of cutaneous squamous cell carcinoma, generally presents as a round erythematous nodule with a central crater filled with keratin. This dermatologic condition more commonly affects adults and is found on sun-exposed areas of the body, such as the face, ears and hands.
D) Superficial folliculitis, an inflammation of hair follicles that can be bacterial in etiology, often incited by Staphylococcus aureus, generally presents as pruritic and tender erythematous follicular-oriented papules and pustules. Folliculitis can affect all age groups and commonly occurs on scalp, beard, trunk, buttocks and thighs.
E) Verruca vulgaris (common warts), a cutaneous manifestation of the human papilloma virus, generally present as hyperkeratotic, verrucous papules with pinpoint black dots visible on the surface, signifying thrombosed capillaries. These lesions present most commonly on the fingers, dorsal hands, elbows and knees.
Molluscum Contagiosum
Surav Man Sakya, BS; Alexandra Flamm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD
A 5-year-old female with no significant past medical history was brought in by her mother who noticed multiple, painless, skin-colored, pearly papules with central umbilication (inlet on right showing enlarged graphical representation of the papules) on her daughter’s right lower abdomen. She was seen scratching the papules while her mother was dressing her. Her immunizations are up to date. She is at 50th percentile for height and weight. She attends a dance class where another child was reported to have similar lesions. On physical exam, multiple, nontender, skin-colored, dome-shaped papules with central umbilication are seen on the right lower abdomen. Remainder of the exam was unremarkable. The diagnosis of molluscum contagiosum was made clinically and no treatment was recommended due to its self-limiting nature.
Molluscum contagiosum (MC) is a localized skin infection caused by the molluscum contagiosum virus, a DNA poxvirus. MC commonly affects children under five years of age and immunocompromised adults. Other risk factors include warm and hot climates and atopic dermatitis.[1] This dermatologic condition generally presents as 2-5 mm, nontender, pink, pearly, dome-shaped papules with central umbilication on the face, trunk and intertriginous areas. However, in immunocompromised individuals, more diffused, 5-10 mm papules are seen.[2] The virus is commonly spread via skin-to-skin contact, autoinoculation and fomites. Diagnosis is generally made clinically, and biopsy may show viral particles in Henderson-Patterson (molluscum) bodies, which are keratinocytes with eosinophilic intracytoplasmic inclusions. This condition is self-limiting and tends to heal without scarring within months to years. However, if desired, removal can be performed via destructive modalities including cryotherapy, curettage and laser therapy. Topical treatment options include cantharidin, retinoids and imiquimod and have variable efficacy. Lastly, oral cimetidine has also shown some benefit in children.[1,3]
References:
- Alikhan A, Hocker TLH. Review of Dermatology. Elsevier - Health Sciences Division; 2016.
- Rosner M, Zloto O. Periocular molluscum contagiosum: six different clinical presentations. Acta Ophthalmol. 2018;96(5):e600-e605.
- Molluscum Contagiosum. CDC. Retrieved from https://www.cdc.gov/poxvirus/molluscum-contagiosum/index.html.
Click here to see older posts.
Image Challenge: Week 8 - Friday, May 29, 2020

A 28-year-old G0 female using intrauterine device for contraception presented with a one-day history of mildly tender, burning blisters on her right superior medial thigh. On exam, she has grouped vesicles on an erythematous base in two clusters, as shown. Prior to the vesicular rash, the patient noticed tingling and hyperesthesia. This past year, she has been in four sexual relationships with inconsistent condom use and endorses two episodes of similar blisters in this region in the past 12 months. She has no prior history of sexually transmitted infections. What is the most likely diagnosis?
A. Chancroid (Haemophilus ducreyi)
B. Genital Herpes (Herpes Simplex Virus Type 2)
C. Granuloma Inguinale (Klebsiella granulomatis)
D. Herpes Zoster (Varicella Zoster Virus)
E. Primary Syphilis (Treponema pallidum)
Correct Answer: B) Genital Herpes (Herpes Simplex Virus Type 2)
Incorrect Answers:
A) Chancroid is caused by Haemophilus ducreyi and generally presents as painful, deep and purulent ulcers with ragged borders.
C) Granuloma inguinale is caused by Klebsiella granulomatis and generally presents as painless ulcer with friable, beefy-red, hypertrophic granulation tissue.
D) Herpes zoster, commonly known as shingles, is a painful viral condition caused by the reactivation of the varicella zoster virus (chickenpox virus). Herpes zoster is characterized by 1-2 days of prodrome symptoms followed by eruption of vesicles with a red base in various stages of healing in an unilateral dermatome distribution.
E) Syphilis is caused by Treponema pallidum, and in the primary stage, it presents as a painless, well-defined and indurated ulcer.
Herpes Simplex Virus (HSV)
Surav Man Sakya, BS; Alexandra Flamm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD
A 28-year-old G0 female using intrauterine device for contraception presented with a one-day history of mildly tender, burning blisters on her right superior medial thigh. On exam, she has grouped vesicles on an erythematous base in two clusters, as shown. Prior to the vesicular rash, the patient noticed tingling and hyperesthesia. This past year, she has been in four sexual relationships with inconsistent condom use and endorses two episodes of similar blisters in this region over the past 12 months. She has no prior history of sexually transmitted infections. She denies vaginal discharge, dysuria and fever. On physical exam, tender vesicles with an erythematous base in two grouped clusters were present on the right superior medial thigh. The first cluster of vesicles is 1 cm in diameter, and the second cluster measures 2 cm in diameter. Diagnosis of recurrent genital herpes simplex virus (HSV type 2) was made based on her history and physical exam. The PCR test later confirmed this diagnosis. The patient reported resolution of the symptoms with valacyclovir 500mg po twice daily for three days and was advised to continue regular follow-ups with dermatology.
Herpes simplex virus infection is caused by herpes simplex virus type 1 (HSV-1) and herpes simplex virus type 2 (HSV-2). The clinical presentations for both viruses are similar; they are grouped vesicles with an erythematous base. The vesicles usually re-epithelialize and heal with crusting.[1] However, common locations of clinical presentation and transmission vary between the two types. HSV-1, a common virus associated with cold sores, typically presents in the oral areas, including the lips. HSV-1, which commonly occurs in childhood, is transmitted via respiratory secretions and saliva. HSV-2, commonly referred to as genital herpes, is found on external genitalia, vagina, cervix, buttocks and perineum in women. Diagnosis is usually clinical, but viral cultures, PCR or Tzanck smears for acute lesions can be done.[2] For primary outbreaks, acyclovir (400mg po TID), famciclovir (250mg po TID) or valacyclovir (1000mg po BID) for seven to ten days may reduce pain and healing time. Moreover, episodic or suppressive therapeutic options exist for treating recurrent infections. For immunocompetent individuals with less than six outbreaks a year, episodic therapy is recommended for convenience and cost. This option recommends acyclovir (800mg po TID for two days), famciclovir (1000mg po BID for a day) or valacyclovir (500mg po BID for three days) within first 24 hours of the prodromal stage. However, for immunocompromised individuals with frequent relapsing genital herpes simplex infections need suppressive therapy, which consists of acyclovir (400mg po twice daily), famciclovir (250mg po twice daily) or valacyclovir (500mg po daily).[3]
References:
- Marks J G, Miller J J. Lookingbill and Marks Principles of Dermatology. Philadelphia: Elsevier. 2019.
- Alikhan A, Hocker TLH. Review of Dermatology. Elsevier - Health Sciences Division; 2017.
- Albrecht M. (2019). Treatment of genital herpes simplex virus infection. UpToDate. Retrieved from http://www.uptodate.com/home/index.html.
Image Challenge: Week 7 - Friday, May 22, 2020

A 43-year-old female with a BMI of 34 (Obese Class 1) presents with hard, painful lumps under the right axilla. She has had reoccurring pus drainage and scarring on the right and left axillae for the past 12 years, but the symptoms have significantly worsened within the last year. She rates her pain 7 out of 10. The pain worsens from extensive chafing while exercising. On physical exam, draining nodules with sinus tract formation (black arrow) on the right axilla are seen. What is the most likely diagnosis?
A. Botryomycosis
B. Hidradenitis suppurativa
C. Lymphogranuloma venereum
D. Nocardiosis
E. Pilonidial cyst
Correct Answer: B) Hidradenitis suppurativa
Incorrect Answers:
A) Botryomycosis is a chronic granulomatous inflammatory process in response to bacterial infection most commonly by Staphylococcus aureus and Pseudomonas aeruginosa. This condition presents with subcutaneous nodules, nonhealing ulcers and sinus tracts caused by the inoculation of bacteria. Common locations of these lesions include the tongue, nasal septum, forehead and scalp.
C) Lymphogranuloma venereum is a venereal disease caused by Chlamydia trachomatis (Serotypes L1-3) most commonly in Asia, Africa and South America and involves males more than females. This condition presents in three stages. Stage 1 of the disease starts with a painless ulcer with lymphangitis. Stage 2 presents with buboes which are unilateral, painful erythematous inguinal lymph nodes. There can be drainage in this stage with pus and sinus tracts. Stage 3 leads to perirectal abscesses, fistulas and stricture. Treatment involves eliminating the infection with doxycycline for 21 days.
D) Nocardiosis is an infection by the bacterial species Nocardia, which is found in soil. Nocardiosis may present systemically or as a cutaneous infection. The cutaneous infection presents in three different forms; actinomycotic mycetoma, lymphocutaneous, and superficial cutaneous. Actinomycotic mycetoma is the most common form occurring due to traumatic inoculation leading to a growing painless nodule with drainage and sinus tract formation. Sulfonamide antibiotics is usually the first line treatment.
E) Pilonidal cyst is a painful draining sinus that occurs in the sacrococcygeal region of the body. This condition usually affects males greater than females. Associated risk factors include curly hair, obesity, poor hygiene and prolonged sitting. Surgical excision is the primary treatment, and oral antibiotics if inflamed due to secondary infection.
Hidradenitis Suppurativa (HS)
Surav Sakya, BS; Alexandra Flamm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD
A 43-year-old female with a BMI of 34 (Obese Class 1) presents with hard, painful lumps under the right axilla. She has had reoccurring pus drainage and scarring on the right and left axillae for the past 12 years, but the symptoms have significantly worsened within the last year. She rates her pain 7 out of 10. The pain worsens from extensive chafing while exercising. On physical exam, draining nodules with sinus tract formation on the right axilla are seen. The pus-filled nodules, sinus tracts and mild scarring suggest Hurley Stage II. Patient is diagnosed with hidradenitis suppurativa. She is prescribed oral doxycycline for 16 weeks. On return to the clinic, the pus drainage has improved from her right axilla, but the pain has not completely resolved.
Hidradenitis Suppurativa (HS), formerly called acne inversa is a devastating chronic inflammatory follicular skin disease that usually starts after puberty, with higher risk of development amongst African Americans and women.[1] HS affects primarily apocrine gland associated areas of the body, which include the axilla, groin, inframammary, and anogenital regions. Clinically, HS usually begins with multiple painful inflammatory nodules and sterile abscesses, which tend to reoccur. Development of hypertrophic scars, sinus tracts (superficial sinus tracts present as double-ended comedones) and contractures may occur during later stages of the disease. In certain cases, thick malodourous viscous suppurative discharge may present with superimposed secondary infection. Other systemic complications may develop including anemia, secondary amyloidosis, lymphedema, fistula formation and squamous cell carcinoma. Suppurative folliculitis with abscess formation, follicular plugging, granulation tissue and fibrosis is seen in apocrine glands on histopathology. The pathophysiology of HS is still largely unknown, but there are a few theories. One is the initial follicular occlusion which triggers an innate and adaptive improper immune response.[2] Secondly, there are mutations associated with gamma-secretase, a protease that cleaves different proteins such as amyloid precursor protein (APP) and Notch signaling pathway proteins involved in gene regulation.[3] Smoking, obesity, metabolic syndrome and depression are risk factors that may be contributory to the development of HS. Multiple grading scales for HS have been developed, and the Hurley Criteria is the most commonly used in clinics. The Hurley Criteria stratifies HS by severity in stages. Hurley Stage I presents with inflamed lesions without scarring. Stage II has scars, inflamed nodules and tunnels. Stage III presents with coalescent lesions with nodules and scars. There are multiple different modalities of treatment that may be used, none of which are which are curative. Treatment options include weight loss, reduction of friction/moisture, antibiotics, such as clindamycin and systemic corticosteroids. Some treatments used for severe disease include medical options of isotretinoin, finasteride, cyclosporin, and TNF-a inhibitors and surgical options.[1]
References:
- Alikhan, A., Hocker, T. Review of Dermatology. Elsevier - Health Sciences Division; 2017.
- Alikhan, A., Sayed, C., Alavi, A., Alhusayen, R., Brassard, A., Burkhart, C., Crowell, K., Eisen, D. B., Gottlieb, A. B., Hamzavi, I., Hazen, P. G., Jaleel, T., Kimball, A. B., Kirby, J., Lowes, M. A., Micheletti, R., Miller, A., Naik, H. B., Orgill, D., & Poulin, Y. (2019). North American clinical management guidelines for hidradenitis suppurativa: A publication from the United States and Canadian Hidradenitis Suppurativa Foundations: Part I: Diagnosis, evaluation, and the use of complementary and procedural management. J Am Acad Dermatol, 81(1), 76-90. https://doi.org/10.1016/j.jaad.2019.02.067
- Notch Signaling. (2020). Cell Signaling Technology. https://www.cellsignal.com/contents/science-cst-pathways-developmental-biology/notch-signaling/pathways-notch
Image Challenge: Week 6 - Friday, May 15, 2020
A 35-year-old, Spanish immigrant male with no significant past medical history presented with small, mildly pruritic, pink follicular papules scattered throughout his upper arms. He stated that his symptoms had been persistent since he was 22. He observed that increased blood flow and sweating after exercises make these signs and symptoms worse. He endorsed a similar condition in his father. What is the most likely diagnosis?
A) Acne vulgaris
B) Keratosis pilaris
C) Milia
D) Phrynoderma
E) Psoriasis
Correct Answer: B) Keratosis pilaris
Incorrect Answers:
A) Acne vulgaris can appear on various parts of the body, but is more commonly seen on the face, neck and upper chest. Although multifactorial in etiology, acne vulgaris can be caused by Cutibacterium acnes. This condition generally presents as open or closed comedones that may progress to more inflammatory papules, pustules, nodules and cysts.
C) Milia are small, white, smooth papules commonly on the nose, chin and cheeks. These are considered to be epidermal inclusion cysts, whose etiology is the infundibula of pilosebaceous follicles. This dermatologic condition is painless and not itchy; most resolve in a couple of days to weeks.
D) Phrynoderma, a cutaneous manifestation of Vitamin A deficiency, generally presents as keratotic follicular papules resembling toad-skin. Vitamin A deficiency also commonly results in ophthalmologic findings, such as blindness, xeropthalmia and bitot spots.
E) Psoriasis most commonly presents as well-demarcated red papules and plaques with white scale. This dermatologic condition is commonly found on elbows, knees, hands, feet and scalp.
Keratosis Pilaris
Surav Man Sakya, BS; Alexandra Flamm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD
A 35-year-old, Spanish immigrant male with no significant past medical history presented with small, mildly pruritic, pink follicular papules scattered throughout his upper arms. He stated that his symptoms had been persistent since he was 22. He observed that increased blood flow and sweating after exercises make these signs and symptoms worse. He endorsed a similar condition in his father. On physical exam, multiple, pink hyperkeratotic papules are distributed on extensor surfaces of the proximal upper extremities bilaterally. A diagnosis of keratosis pilaris is made clinically. Exfoliation of the affected area and several over-the-counter lotions containing lactic acids, salicylic acids and urea are recommended. On a return visit several months later, he endorsed mild improvement without complete resolution of symptoms.
Keratosis pilaris, colloquially known as ‘KP’ and ‘chicken skin’, is caused by abnormal keratinization of hair follicles. This dermatologic condition typically presents during childhood and may affect 25 to 60% of adolescents and adults. KP, commonly found on cheeks, upper arms, thighs, and buttocks, is characterized by multiple, small, spiny keratotic papules ranging in color from skin-colored to pink. Several epidemiology studies showed that KP is the most common pediatric follicular disorder.1 Moreover, there is a higher reported prevalence among the British and Indian populations. KP has a strong association with atopic dermatitis, ichthyosis vulgaris and xerosis; obesity, diabetes and pregnancy have also been implicated in the pathogenesis of KP.1 On histology, keratotic plugging of the pilosebaceous follicles can be seen. KP and its subtypes have been noted to have a potential genetic etiology, and KP has been linked to genetic syndromes, such as Down syndrome. Medications that have been shown to cause KP-like lesions include cyclosporine, B-Raf inhibitors and tyrosine kinase inhibitors. KP can improve spontaneously; however, for treatment, topical agents including lactic acids, salicylic acids, urea, retinoids, calcineurin inhibitors and petroleum ointment have shown variable successes. As KP can be difficult to treat, another management option is to use cosmetics to camouflage the affected areas.2
References:
1.Wang JF, Orlow SJ. Keratosis Pilaris and its Subtypes: Associations, New Molecular and Pharmacologic Etiologies, and Therapeutic Options. American Journal of Clinical Dermatology. 2018;19(5):733-757.
2.Alikhan A, Hocker TLH. Review of Dermatology. Elsevier - Health Sciences Division; 2017.
Image Challenge: Week 5 - Friday, May 8, 2020

A 26-year-old Asian female with no significant past medical history presented with a large, red, pruritic, plaque on her right thigh for 12 hours. She endorses 3/10 pain when she scratches it. Yesterday, she went hiking with her friends. She first noticed a small red bump that was itchy. Within hours, the redness around the bump grew. She applied ice to relieve the swelling, and anti-itch spray with hydrocortisone that did not help. She denies any headache, fever or chills. She experienced similar reactions in the past after hiking that gradually improved over the next several days. Which of the following is the most likely causal organism/vector?
A) Bed bugs (Cimex lectularius)
B) Brown recluse spider (Loxosceles reclusa)
C) Dermatophyte (Trichophyton rubrum)
D) Mosquito (Culex pipiens)
E) Tick (Ixodes scapularis)
F) Group A Streptococcus (Streptococcus pyogenes)
Correct Answer D) Mosquito (Culex pipiens)
Incorrect Answers:
A) When bitten, bed bugs (Cimex lectularius) may cause a hypersensitivity reaction because their saliva contains nitrophorin, an immunogenic hemoprotein. This generally presents with multiple urticarial papules with possible erythema, edema and itching. The cutaneous papules have a grouped distribution in the “breakfast, lunch and dinner” pattern.
B) Brown recluse spider (Loxosceles reclusa) may cause a necrotic reaction with eschar formation at the site of the bite. The bite is painless, but further complications include ischemia and thrombosis. The toxins that cause the reaction are sphingomyelinase D and hyaluronidase.
C) Trichophyton rubrum is the most common causal organism of tinea corporis, a dermatophyte infection. Tinea corporis usually presents as scaly annular patches and plaques with inflamed, palpable borders.
E) Erythema migrans is a cutaneous manifestation of Lyme disease that occurs in 90% of individuals bitten by the Ixodes tick, a vector for the spirochete, Borrelia burgdorferi. The tick generally attaches for >1 day, and the large, red annular skin finding, commonly described as a “bull’s eye” presents after 7 to 15 days. Lyme disease generally presents early with flu-like symptoms and lymphadenopathy while Bell’s palsy, arthralgias, and AV heart block may present later.
F) Streptococcus pyogenes is the most common causal organism of cellulitis, an erythematous and tender skin lesion with ill-defined margins. Individuals may have lymphadenitis and other systemic symptoms such as fever, chills and confusion.
Mosquito Bite Hypersensitivity
Surav Man Sakya, BS; Alexandra Flamm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD
A 26-year-old Asian female with no significant past medical history presented with a large, red, pruritic, plaque on her right thigh for 12 hours. She endorses 3/10 pain when she scratches it. Yesterday, she went hiking with her friends. She first noticed a small red bump that was itchy. Within hours, the redness around the bump grew. She applied ice to relieve the swelling, and anti-itch spray with hydrocortisone that did not help. She denies any headache, fever or chills. She experienced similar reactions in the past after hiking that gradually improved over the next several days. On physical exam, a 12-cm, well-circumscribed, erythematous plaque, consistent with a wheal-and-flare reaction, was observed on her right thigh with mild pain on palpation. Insect bite hypersensitivity diagnosis was made. After 7 days, her condition resolved without complications.
Insect bites result in different type and degree of severity of hypersensitivity reaction. Most common type is immediate, IgE-mediated type I hypersensitivity characterized by immune reaction occurring within minutes to hours. Antigen exposure causes release of IgE antibodies that can cause cell degranulation and histamine release. Moreover, sensitization with preformed IgE antibodies is seen. Another common type is delayed, T-cell-mediated type IV hypersensitivity that requires days before any signs and symptoms. Moreover, T-cell sensitization releasing cytokines can occur in subsequent exposures.1 Although most insect bites are mild and self-limiting, some experience more severe reaction to them. Skeeter syndrome is a large local skin reaction occurring within 8 to 12 hours to mosquito bites in individuals with allergic predisposition.2 Skeeter syndrome usually presents with an itchy, painful area of erythema, swelling and induration that can be larger than 10 cm in diameter. Some patients may experience fever, but the skin finding is self-limiting within 3 to 10 days. This reaction may be caused by a combination of type I and IV hypersensitivity. This syndrome is commonly seen in individuals in mosquito endemic areas, exposed to outdoor environments and with mosquito bite sensitization without forming natural immunity. Treatment includes supportive care, antihistamines, or oral glucocorticoids for severe reactions. Prevention of bites is helpful and includes protective clothing and insect repellent.
References:
1. Pali-Scholl I, Blank S, Verhoeckx K, et al. EAACI position paper: Comparing insect hypersensitivity induced by bite, sting, inhalation or ingestion in human beings and animals. Allergy. 2019;74(5):874-887.
2. Simons FE, Peng Z. Skeeter syndrome. J Allergy Clin Immunol. 1999;104(3 Pt 1):705-707.
3. Alikhan A, Hocker TLH. Review of Dermatology. Elsevier - Health Sciences Division; 2017.
Image Challenge: Week 4 - Friday, May 1, 2020


A 53-year-old Asian female with no significant past medical history presented with a progressive hair loss on the scalp over the past several years. Initially, she had areas of thinner hair on the top and crown of the head. Over the years, she also observed a widening of the center hair part from increased hair loss and thinning. She endorsed a similar hair loss in a frontotemporal pattern in her father whose first occurrence was in his 20s. In the clinic, hair pull test was negative. What is the most likely diagnosis?
A) Alopecia areata
B) Anagen effluvium
C) Androgenetic alopecia
D) Telogen effluvium
E) Trichotillomania
Correct Answer: C) Androgenetic alopecia
Incorrect Answers:
A) Alopecia areata (AA) is an acquired, circumscribed, non-scarring hair loss caused by cytotoxic T-cells attacking the hair follicle antigens. This autoimmune condition generally presents as well-demarcated, round patches of hair loss on the scalp. AA is commonly seen in individuals under 30 years of age and may be associated with other autoimmune diseases, such as thyroid dysfunction, type 1 diabetes mellitus, Addison’s disease, pernicious anemia, systemic lupus erythematosus, rheumatoid arthritis, psoriasis and vitiligo. On physical exam, short, “exclamation point” hairs on the edges of the patches can be seen.
B) Anagen effluvium is a diffuse, non-scarring alopecia that is most commonly seen as a side effect of chemotherapy. Unlike telogen effluvium, it is characterized by rapid hair loss. This condition usually occurs within 2 weeks of starting chemotherapy because of the rapid cessation of hair cell division. This condition is reversible with most chemotherapy drugs.
D) Telogen effluvium is a reversible, diffuse, non-scarring alopecia that can be triggered by hormonal imbalance, nutritional deficiency, drug use and stress. This dermatologic condition results in increased hair loss (>150 hairs/day; Normal: 100-150 hairs/day) and decreased density of scalp hair because more hairs shift into the telogen phase. The hair pull test is positive (4-6 hairs pulled out of 50). Unlike anagen effluvium, the condition usually occurs 2 to 4 months after starting medications such as heparin, beta-blocker, interferon, lithium and retinoids. Other reversible stressors include pregnancy, thyroid disease, malnutrition and hospitalization/surgery.
E) Trichotillomania (TTM) is an impulse control disorder in which individuals fail to resist urges to pull out their own hair. Onset of TTM, which occurs predominantly in women, appears to be mostly in childhood or adolescence. It is associated with significant functional impairment and psychiatric comorbidity, such as obsessive-compulsive disorder. TTM can involve multiple sites, although it is usually confined to one or two sites. The scalp is the most common hair pulling site, followed by the eyebrows and eyelashes. On physical exam, large, irregular patches of hair loss can be seen. Hair length may vary because hairs may not be pulled out at random but can be chosen based on certain characteristics, such as hair of a certain color, length or texture.
Androgenetic Alopecia (AGA)
Surav Man Sakya, BS; Alexandra Flamm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD
A 53-year-old Asian female with no significant past medical history presented with a progressive hair loss on the scalp over the past several years. Initially, she had areas of thinner hair on the top and crown of the head. Over the years, she also observed a widening of the center hair part from increased hair loss and thinning. She endorsed a similar hair loss in a frontotemporal pattern in her father whose first occurrence was in his 20s. On physical exam, her hair is diffusely fine, and hair loss is most evident at the vertex of her scalp with progressive hair thinning toward the frontal scalp. There is a significant widening of the midline part and noticeable decrease in hair volume, which is consistent with Type 2 (moderate) Ludwig classification. In the clinic, hair pull test was negative. The diagnosis of androgenetic alopecia was made clinically, and 5% topical minoxidil foam applied twice daily was recommended. On a return visit several months later, she endorsed mild slowing of the rate at which she was losing hair, but no significant regrowth of hair.
Androgenetic alopecia (AGA), commonly called female/male pattern baldness, is an acquired, diffuse, non-scarring hair loss affecting 80% of men and 50% of women by age 70. There is a strong genetic predisposition, and many believe that dihydrotestosterone (DHT), a derivative of testosterone acts on the hair follicles and causes hair loss. AGA presents differently between men and women. In men, there is a bitemporal ‘M’ pattern of hairline recession, and in women, there is a progressive hair thinning from the vertex without affecting the frontal hairline. Microscopically, there is an increase in vellus and miniaturized hairs and decrease in terminal (long, thick and deeply pigmented) hairs. First-line treatment for men is oral finasteride and 5% topical minoxidil. In women, 5% topical minoxidil is recommended. These are FDA approved treatment options to slow hair loss and stimulate hair growth. Minoxidil, a vasodilator, increases blood flow to the hair cells to promote the anagen (growth) hair phase. Finasteride, a 5a-reductase inhibitor, prevents testosterone conversion to DHT. Moreover, other treatment options include oral anti-androgen drugs, such as spironolactone, platelet-rich plasma (PRP) injections and hair transplant surgery. A popular management option is to use cosmetics or hair wigs to camouflage the hair loss and thinning. Sun protection is also crucial because the bald areas have a greater propensity to incur sun damage.1
Reference:
1. Alikhan A, Hocker TLH. Review of Dermatology. Elsevier - Health Sciences Division; 2017.
Image Challenge: Week 3 - Friday, April 24, 2020

A 25-year-old South Asian female with no significant past medical history presented with finely scaling hyper- and hypopigmented macules coalescing into large patches over her upper and mid back. She stated that her symptoms had been persistent for the past five years. She observed that humid summers and exercise make these signs and symptoms worse. She tried scrubbing her back with an exfoliating washcloth, but it did not change the appearance and itchiness. The diagnosis was confirmed by potassium hydroxide (KOH) preparation of the skin scrapings, which demonstrated the characteristic “spaghetti and meatballs” appearance. Which of the following is the most likely causal organism for her diagnosis?
A) Candida albicans
B) Cutibacterium acnes
C) Malassezia globosa
D) Sporothrix schenckii
E) Trichophyton rubrum
Correct Answer: C) Malassezia globosa
Incorrect Answers:
A) Candida albicans, most commonly found in the normal flora of the skin and digestive tracts, causes localized and systemic candidiasis. Severity of signs and symptoms depends on the health status of the individual. Candidiasis of the skin generally presents in skinfolds as pruritic, beefy red color rash with satellite papules and pustules. In immunocompromised individuals, systemic involvement of various organ systems can be seen. Microscopically, the KOH examination reveals yeasts and pseudohyphae.
B) Cutibacterium acnes (formerly known as Propionibacterium acnes) is seen in acne vulgaris, which predominantly affects individuals of 11 to 30 years of age. Acne vulgaris can appear on various parts of the body, but is more commonly seen on the face, neck and upper chest. This condition generally presents as open or closed comedones that may progress to more inflammatory papules, pustules, nodules and cysts. On histology, these follicles are filled with laminated keratin and debris.
D) Sporothrix schenckii causes sporotrichosis, a fungal infection that is characterized by multiple, ascending ulcerated nodules and subcutaneous abscesses, often following a lymphatic distribution of spread. Sporotrichosis usually presents in gardeners and farmers, as these organisms living on dead and decaying organic matter can be inoculated through trauma. Microscopically, cigar-shaped budding yeasts are visualized.
E) Trichophyton rubrum is the most common cause of tinea corporis, a dermatophyte infection. Tinea corporis usually presents as scaly annular patches and plaques with inflamed, palpable borders. On histology and KOH, this dermatologic condition can be distinguished from tinea versicolor by their longer branching hyphae and lack of spore-like structures.
Tinea Versicolor/Pityriasis Versicolor
Surav Man Sakya, BS; Alexandra Flamm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD
A 25-year-old South Asian female with no significant past medical history presented with finely scaling hyper- and hypopigmented macules coalescing into large patches over her upper and mid back. She stated that her symptoms had been persistent for the past five years. She observed that humid summers and exercise make these signs and symptoms worse. She tried scrubbing her back with an exfoliating washcloth, but it did not change the appearance and itchiness. On physical exam, large, irregular patches with fine scales and with various colors ranging from white to brown to reddish brown were observed on her upper and mid back. The diagnosis of tinea versicolor was made clinically and was confirmed by potassium hydroxide (KOH) preparation of the skin scrapings, which demonstrated the characteristic “spaghetti and meatballs” appearance.
Tinea versicolor/pityriasis versicolor, a superficial fungal disease, is most commonly caused by the overgrowth of Malassezia furfur and Malassezia globosa in healthy individuals of 15 to 24 years of age. These organisms reside as yeast forms in our normal flora, but can transform into filamentous and hyphal forms and infect the stratum corneum. Therefore, the KOH stain under the microscope shows round yeasts resembling “meatballs” and filamentous hyphae resembling “spaghetti”. The predominant risk factors are sun exposure during warm, humid weather, excessive sweating and oily skin. Therefore, tinea versicolor favors areas with sebaceous glands, such as the scalp, face, neck, upper chest and upper back. Along with mild pruritus, this condition is characterized by well-demarcated, hyper- and hypopigmented macules and patches with fine scales. Without treatment, the macules can coalesce into large, irregularly-shaped patches. Tinea versicolor can cause a variety of pigmentary changes including hypopigmentation, hyperpigmentation and erythema. Pityriasis versicolor alba (hypopigmentation) is believed to be due to melanocyte inhibition secondary to azelaic acid production by the Malassezia species, while erythema is from inflammation in this susceptible area. Treatment consists of topical or systemic azole antifungals and selenium sulfide shampoo and lotion. Although these treatment options can cause resolution of symptoms, recurrence is common, and the condition can be chronic. People may experience reduction in quality of life from emotional distress and self-consciousness. One management option is to use cosmetics to camouflage the discoloration. Additionally, since the infected areas do not tan, sunlight exposure or use of tanning bed can cause a more prominent appearance of the discoloration.1
Reference:
- Alikhan A, Hocker TLH. Review of Dermatology. Elsevier - Health Sciences Division; 2016.
Image Challenge Week 2: April 17, 2020

A 21-year-old healthy Brazilian male presented with well-demarcated, white oval macules and patches on his hands, jaw and behind the knees, which he stated as having been present for 3 years. He recalled that the first occurrence on his hands and fingers was sudden and during a stressful period in his life. Since then, he noticed an increase in size and frequency of the depigmentation during times of stress. What is the most likely diagnosis?
A) Idiopathic guttate hypomelanosis
B) Leprosy (Hansen’s disease)
C) Nevus depigmentosus/nevus achromicus
D) Tinea versicolor/pityriasis versicolor
E) Vitiligo
Correct Answer: E) Vitiligo
Incorrect Answers:
A) Idiopathic guttate hypomelanosis generally presents as small, white macules on the forearms and shins and remains stable in size. This condition most commonly affects individuals over 40 and is thought to be a part of the normal aging process.
B) Leprosy (Hansen’s disease) is a mycobacterial infection caused by Mycobacterium leprae. Leprosy involves both the skin and nerves, and the organism grows best in cooler areas, such as the nose, testes and ear lobes and favors peripheral nerves near the skin surface. Primary cutaneous manifestation is characterized by erythematous and/or hypopigmented annular plaques with mild scaling. Moreover, a widespread nerve damage commonly results in ocular damage, stocking-glove anesthesia, neuropathic ulcers and flexural deformities.
C) Nevus depigmentosus/nevus achromicus generally presents as well-demarcated hypopigmented patches that typically appear in infancy. They remain stable in size and distribution throughout life. The histopathology reveals a normal number of melanocytes but a decreased number of melanosomes within the melanocytes.
D) Tinea versicolor/pityriasis versicolor is a superficial fungal disease caused by Malassezia globosa and/or Malassezia furfur. This condition generally presents as hyper- and hypopigmented finely scaling oval macules and patches because Malassezia species produce azelaic acid, which inhibits melanocytes. Tinea versicolor favors areas with sebaceous glands, such as scalp, face, neck, upper chest, and upper and lower back.
Vitiligo
Surav Man Sakya, BS; Alexandra Flamm, MD; Brian Green, DO; Joslyn Sciacca Kirby, MD
A 21-year-old healthy Brazilian male presented with well-demarcated, white oval macules and patches on his hands, jaw and behind the knees. He had no prior medical illness and did not take any medications. The depigmentation suddenly appeared on his hands and fingers during stress when he was 18. Throughout the years, they became greater in size and frequency on his hands and progressed to other parts of his body during times of stress. He denied itching, discomfort and pain. He endorsed a similar condition in his mother whose first occurrence was in her late-teens and in his maternal grandfather. He denied any fatigue, weight changes, polydipsia, polyuria, polyphagia, joint pain and other skin rash. On his physical exam, there were multiple, well-defined white macules and patches on the top of his hands and fingers, jaw and behind the knees. Diagnosis of vitiligo was made clinically, and was given topical corticosteroid cream. He did not experience resolution of the depigmentation after several months. He stopped treatment because he did not see any improvement.
Vitiligo, a multifactorial disorder of hypopigmentation and depigmentation, is caused by decrease in melanin production secondary to melanocyte destruction. This dermatologic condition usually presents around age 20 and may present earlier in females.
Although the exact pathogenesis is unknown, the most accepted is the autoimmune theory of melanocyte destruction by cellular and humoral immunity. Vitiligo, commonly found on hands, axillae, groin and face, is characterized by well-circumscribed, asymptomatic depigmented macules or patches. Incomplete penetrance, genetic heterogeneity and multiple susceptibility loci have been implicated in vitiligo. Vitiligo may be associated with other autoimmune diseases, such as thyroid dysfunction, type 1 diabetes mellitus, Addison’s disease, pernicious anemia, systemic lupus erythematosus, rheumatoid arthritis, psoriasis, alopecia areata and uveitis. Treatment options include topical steroids, topical calcineurin inhibitors, topical vitamin D analogs, NB-UVB phototherapy, immunosuppressants and surgery. These treatment options may help with repigmentation and prevent the spread of vitiligo in some cases. Since vitiligo is difficult to treat, one management option is to use cosmetics to camouflage the depigmented areas. Sun protection in these depigmented areas is crucial because they have a greater propensity to incur sun damage. Moreover, vitiligo is not contagious and is not due to lack of hygiene. People with vitiligo may experience reduction in quality of life and psychosocial well-being from various misconceptions and negative attitudes about vitiligo. Educating the public about vitiligo is important, and for younger individuals with vitiligo, counseling and therapy are recommended.[1]
Reference:
1. Alikhan A, Hocker TLH. Review of Dermatology. Elsevier - Health Sciences Division; 2016.
Image Challenge Week 1: April 10, 2020

A 58-year-old Asian male presented with a 4-day history of a painful, burning rash on his right cheek, chin and postauricular region. What is the diagnosis?
A) Herpes Simplex
B) Impetigo
C) Herpes Zoster
D) Rickettsialpox
E) Variola/ Smallpox
F) Bullous Insect Bite
Correct Answer: C) Herpes Zoster
Incorrect Answers:
A) Herpes Simplex generally presents as grouped/clustered vesicles on erythema base affecting the orolabial (HSV-1) and genital (HSV-2) regions.
B) Impetigo generally presents as erosions with “honey-colored” crusts affecting the perioral and perinasal regions of face.
D) Rickettsialpox generally presents within 48 hours of the mite bite with a papulovesicle at the bite site progressing to an eschar. This is followed by a widespread cutaneous eruption of red macules and papulovesicles with hemorrhagic crusts.
E) Variola/ smallpox generally presents as centrifugal vesiculopustular eruption favoring the face, arms and legs following 1-4 days of prodrome symptoms (fever, headache, myalgias and malaise). All lesions will be in the same stage.
F) Bullous insect bites generally present as multiple tense bullae without significant erythematous and edematous bases.
Herpes Zoster (Shingles)
Surav Sakya, BS, Alexandra Flamm, MD, Brian Green, MD, Joslyn Sciacca Kirby, MD
A 58-year-old Asian male presented with a 4-day history of a painful, burning rash on his right cheek, chin and postauricular region. The patient experienced prodrome symptoms of itching, tingling, hyperesthesia and pain prior to the rash. He denied fever, headache, facial paralysis and any changes in vision, hearing and taste. On physical exam, there were multiple, pruritic vesicles on erythema base in various stages of healing in a C2 and C3 dermatome pattern on the right. Diagnosis of herpes zoster was made clinically, and patient was prescribed valacyclovir 1g TID for 7 days. The patient experienced resolution of rash and blisters, and postherpetic neuralgia improved over the next several weeks. Recommendation for Shingrix was made.
Herpes zoster, commonly known as shingles, is a painful viral condition caused by the reactivation of the varicella zoster virus (chickenpox virus). This dermatologic condition mainly affects the elderly and immunocompromised individuals who had chickenpox in childhood. Herpes zoster is characterized by 1-2 days of prodrome symptoms followed by eruption of vesicles with red base in various stages of healing and in a unilateral dermatome distribution and possible postherpetic neuralgia.[1] The current CDC vaccination recommendation for adult ages 50 years or older is a 2-dose series of RZV (Shingrix) 2-6 month apart regardless of previous herpes zoster or history of ZVL (Zostavax) vaccination. If ages 60 years or older, a 2-dose series of RZV (Shingrix) 2-6 months apart or 1 dose of ZVL (Zostavax) if not previously vaccinated.[2]
References:
1. Alikhan A, Hocker TLH. Review of Dermatology. Elsevier - Health Sciences Division; 2016.
2. “Recommended Adult Immunization Schedule. Shingles (Herpes Zoster) Vaccination” Centers of Disease Control and Prevention (CDC), 2020.
https://www.cdc.gov/.../adult/adult-combined-schedule.pdf